Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Relationship between overweight, obesity and sleep disorders in adolescents from selected cities of Upper Silesia, Poland
1
Chair and Department of Medicine and Environmental Epidemiology, Medical University of Silesia, Katowice, Poland
Corresponding author
Iwona Lizończyk
Chair and Department of Medicine and Environmental Epidemiology, Medical University of Silesia in Katowice, Jordana 19, 41-808, Zabrze, Poland
Chair and Department of Medicine and Environmental Epidemiology, Medical University of Silesia in Katowice, Jordana 19, 41-808, Zabrze, Poland
Ann Agric Environ Med. 2021;28(1):193-197
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Overweight and obesity affect an increasing number of children and adolescents in Poland. This excessive body weight usually coexists with sleep disorders and other afflictions, which is worrisome.
Objective:
The aim of the study was to assess the prevalence of overweight, obesity, and sleep disorders among adolescents and demonstrate their relationships.
Material and methods:
The study included 1,002 students. Nutritional habits and subjective assessment of sleep were evaluated with the author’s survey; daytime sleepiness and sleep quality were assessed with Epworth Sleepiness Scale (ESS) and Sleep Quality Scale (SQS). Statistical calculations were performed with the STATISTICA 12.0 programme.
Results:
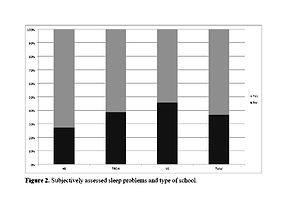
24.7% of adolescents suffered from overweight or obesity, 38% reported sleep problems in subjective assessment, 10.5% exhibited excessive daytime sleepiness, determined by ESS, and 14.3% had impaired quality of sleep as determined by SQS. Gender affected all the discussed problems. Type of school affected all the above, except for daytime sleepiness. In the group with overweight and obesity, 46.6% of individuals reported sleep problems in subjective assessment. About 59.1% of adolescents reported chronic fatigue. Reduced concentration and difficulties in learning were reported in 36.3% of all students, and in 46% of students with overweight and obesity.
Conclusions:
The problem of excess body weight is a very alarming phenomenon since it affects almost 1/4 of the students. Almost half of the students with overweight and obesity reported sleep problems, which is strongly correlated with the type of school. Furthermore, excess body weight influenced the prevalence of reduced concentration and learning difficulties among adolescents.
Overweight and obesity affect an increasing number of children and adolescents in Poland. This excessive body weight usually coexists with sleep disorders and other afflictions, which is worrisome.
Objective:
The aim of the study was to assess the prevalence of overweight, obesity, and sleep disorders among adolescents and demonstrate their relationships.
Material and methods:
The study included 1,002 students. Nutritional habits and subjective assessment of sleep were evaluated with the author’s survey; daytime sleepiness and sleep quality were assessed with Epworth Sleepiness Scale (ESS) and Sleep Quality Scale (SQS). Statistical calculations were performed with the STATISTICA 12.0 programme.
Results:
24.7% of adolescents suffered from overweight or obesity, 38% reported sleep problems in subjective assessment, 10.5% exhibited excessive daytime sleepiness, determined by ESS, and 14.3% had impaired quality of sleep as determined by SQS. Gender affected all the discussed problems. Type of school affected all the above, except for daytime sleepiness. In the group with overweight and obesity, 46.6% of individuals reported sleep problems in subjective assessment. About 59.1% of adolescents reported chronic fatigue. Reduced concentration and difficulties in learning were reported in 36.3% of all students, and in 46% of students with overweight and obesity.
Conclusions:
The problem of excess body weight is a very alarming phenomenon since it affects almost 1/4 of the students. Almost half of the students with overweight and obesity reported sleep problems, which is strongly correlated with the type of school. Furthermore, excess body weight influenced the prevalence of reduced concentration and learning difficulties among adolescents.
REFERENCES (33)
1.
Obesity and overweight [Internet]. World Health Organization. World Health Organization; 2018 [cited 2019 Dec 15]. Available from: https://www.who.int/news-room/....
2.
Ritchie H, Roser M. Obesity [Internet]. Our World in Data. 2017 [cited 2019 Dec 15]. Available from: https://ourworldindata.org/obe....
3.
Piekarzewska M, Wieczorkowski R, Zajenkowska-Kozłowska A. Health status of population in Poland in 2014. CSO, Social Surveys and Living Conditions Department. Warszawa; 2016. Polish.
4.
Mazur J, Małkowska-Szkutnik A. Zdrowie i zachowania zdrowotne młodzieży szkolnej w Polsce na tle wybranych uwarunkowań socjodemograficznych. Wyniki badania HBSC. Instytut Matki i Dziecka. Warszawa; 2014. Polish.
5.
American Academy of Sleep Medicine. International Classification of Sleep Disorders, Third edition. Diagnostic and Coding Manual. 2014.
6.
Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014; 15(12): 1456–62. doi:10.1016/j.sleep.2014.07.018.
7.
Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The Great Sleep Recession: Changes in Sleep Duration Among US Adolescents, 1991–2012. Pediatrics. 2015; 135(3): 460–8. doi:10.1542/peds.2014–2707.
8.
Kronholm E, Puusniekka R, Jokela J, Villberg J, Urrila AS, Paunio T, et al. Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J Sleep Res. 2014 Apr; 24(1): 3–10. https://doi.org/10.1111/jsr.12....
9.
Błońska B, Gotlib J. Występowanie zaburzeń snu wśród studentów. Wydawnictwo UR. 2012;4:487–497. Polish.
10.
Fatima Y, Doi SAR, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015; 16(2): 137–49. https://doi.org/10.1111/obr.12....
11.
Chen T, Wu Z, Shen Z, Zhang J, Shen X, Li S. Sleep duration in Chinese adolescents: biological, environmental, and behavioral predictors. Sleep Med. 2014; 15(11): 1345–53. doi:10.1016/j.sleep.2014.05.018.
12.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002; 11(246): 1–190.
13.
Murray MW. A new method for measuring daytime sleepiness scale. Sleep. 1991; 14: 540–545. doi:10.1093/sleep/14.6.540.
14.
Kasperczyk J, Jośko J. The estimation of sleep quality by means of SEN questionnaire. Środowiskowe źródła zagrożeń zdrowotnych. Wydawnictwo Polihymnia. Lublin;2007:225–227.
15.
About the ESS [Internet]. Epworth Sleepiness Scale. [cited 2019 Dec 15]. Available from: http://epworthsleepinessscale.....
16.
Höglund A, Hagell P, Broman J, Pålhagen S, Sorjonen K, Fredrikson S. A 10-year follow-up of excessive daytime sleepiness in Parkinson’s Disease. Parkinsons Dis. 2019; 2019:1–7. doi:10.1155/2019/5708515.
17.
Kułaga Z, Różdżyńska-Świątkowska A, Grajda A, Gurzkowska B, Wojtyło M, Góźdź M et al. Siatki centylowe dla oceny wzrastania i stanu odżywienia polskich dzieci i młodzieży od urodzenia do 18 roku życia. Stand Med, Pediatr. 2015; 12: 119–135. Polish.
18.
Malczyk E. The review of research methods used to assess nutritional status of children and youth in Poland in period 2005–2015. Ann Acad Med Siles. 2016; 70: 80–83. Polish. doi:10.18794/aams/58972.
19.
Luyster FS, Choi J, Yeh C-H, Imes CC, Johansson AE, Chasens ER. Screening and evaluation tools for sleep disorders in older adults. Appl Nurs Res. 2015; 28(4): 334–40. doi:10.1016/j.apnr.2014.12.007.
20.
Lau K, Jośko J. Zaburzenia snu jako problem zdrowia publicznego. Zdr Publ. 2010; 120(2): 199–202. Polish.
21.
Verkooijen S, Vos ND, Bakker-Camu BJ, Branje SJ, Kahn RS, Ophoff RA, et al. Sleep Disturbances, Psychosocial Difficulties, and Health Risk Behavior in 16,781 Dutch Adolescents. Acad Pediatr. 2018; 18(6): 655–61. doi:10.1016/j.acap.2018.03.003.
22.
Kasperczyk J, Jośko J, Cichoń-Lenart A, Lenart J. Epidemiologia zaburzeń snu u młodzieży mieszkającej na Górnym Śląsku. Sen. 2006; 6(1): 8–13. Polish.
23.
Lehnkering H, Siegmund R. Influence of chronotype, season, and sex of subjects on sleep behavior of young adults. Chronobiol Int. 2007; 24: 875–888. doi:10.1080/07420520701648259.
24.
Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, Chang CJ. The association between self-reported sleep quality and overweight in a Chinese population. Obesity. 2013; 21(3): 486–92. doi:10.1002/oby.20259.
25.
Sadowska J, Daniel I. Konsekwencje zdrowotne nieprawidłowości w żywieniu dzieci i młodzieży w wieku gimnazjalnym. Kosmos. Problemy nauk biologicznych. 2016; 65(4): 553–561. Polish.
26.
Bonuck K, Chervin RD, Howe LD. Sleep-disordered breathing, sleep duration, and childhood overweight: a longitudinal cohort study. J Pediatr. 2015; 166(3): 632–639. doi:10.1016/j.jpeds.2014.11.001.
27.
Peltzer K, Pengpid S. Sleep duration, sleep quality, body mass index and waist circumferences among young adults from 24-low and middle-income and two high-income countries. Int J Environ Res Public Health. 2017; 14(6). doi:10.3390/ijerph14060566.
28.
Burt J, Dube L, Thibault L, Gruber R. Sleep and eating in childhood: a potential behavioral underlying the relationship between poor sleep and obesity. Sleep Med. 2014; 15(1): 71–75. doi:10.1016/j.sleep.2013.07.015.
29.
He F, Bixler EO, Liao J, Berg A, Imamura Kawasawa Y, Fernandez-Mendoza J et al. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015; 16(12): 1489–1494. doi:10.1016/j.sleep.2015.07.028.
30.
Grandner M, Seixas A, Shetty S, Shenoy S. Sleep Duration and Diabetes Risk: Population Trends and Potential Mechanisms. Curr Diab Rep. 2016; 16(11). doi:10.1007/s11892–016–0805–8.
31.
Stalmach M, Jodkowska M, Radiukiewicz K, Oblacińska A. Sleep duration among students and its association with health behaviors. Hygeia Public Health. 2016; 51(2): 179–186. Polish.
32.
Khan MK, Chu YL, Kirk SF, Veugelers PJ. Are sleep duration and quality associated with diet quality, physical activity, and body weight status? A population-based study of Canadian children. Can J Public Health. 2015; 106(5): 277–282. doi:10.17269/cjph.106.4892.
33.
Lu Q, Hou F, Sun Y, Zhang Z, Tao F. Relations between duration of sleep, dietary patterns and the prevalence of overweight/obesity among 11–13 year-olds in Xuzhou, Jiangsu province of China. Zhonghua Liu Xing Bing Xue Za Zhi. 2014; 35(4): 381–385.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.