Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Relationship between concentration of air pollutants and frequency of hospitalisations due to respiratory diseases
1
Chair and Department of Pneumonology, Oncology and Allergology, Medical University, Lublin, Poland
2
Department of Pharmaceutical Botany, Medical University, Lublin, Poland
3
Second Department of Radiology, Medical University, Lublin, Poland
Corresponding author
Anna Grzywa-Celińska
Chair and Department of Pneumonology, Oncology and Allergology, Medical University of Lublin, ul. Jaczewskiego 8, 20-954, Lublin, Poland
Chair and Department of Pneumonology, Oncology and Allergology, Medical University of Lublin, ul. Jaczewskiego 8, 20-954, Lublin, Poland
Ann Agric Environ Med. 2024;31(1):13-23
KEYWORDS
TOPICS
- Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)
- Health effects of chemical pollutants in agricultural areas , including occupational and non-occupational effects of agricultural chemicals (pesticides, fertilizers) and effects of industrial disposal (heavy metals, sulphur, etc.) contaminating the atmosphere, soil and water
ABSTRACT
Introduction and objective:
Smog, which contains fine dusts, non-metal oxides, metals and organic compounds can have irritating, allergenic and immunomodulatory effects leading to the development of respiratory diseases and their exacerbations. The aim of the study was to search for a relationship between concentrations of air pollutants and the frequency of hospitalizations due to exacerbation of asthma, chronic obstructive pulmonary disease, or abnormalitis in breathing.
Material and methods:
Hospital admission data was accessed from the hospital digital in-formation system. From the publicly available database of the Chief Inspectorate for Environmental Protection, data concerning the concentrations of pollutants, such as PM2.5 and PM10, sulphur oxide IV (SO2), nitric oxide IV (NO2), carbon monoxide II (CO), benzene and ozone (O3), measured daily with hourly accuracy was used. The results of the average concentrations of air pollutants were compared with the rates of hospitalization in the corresponding time intervals.
Results:
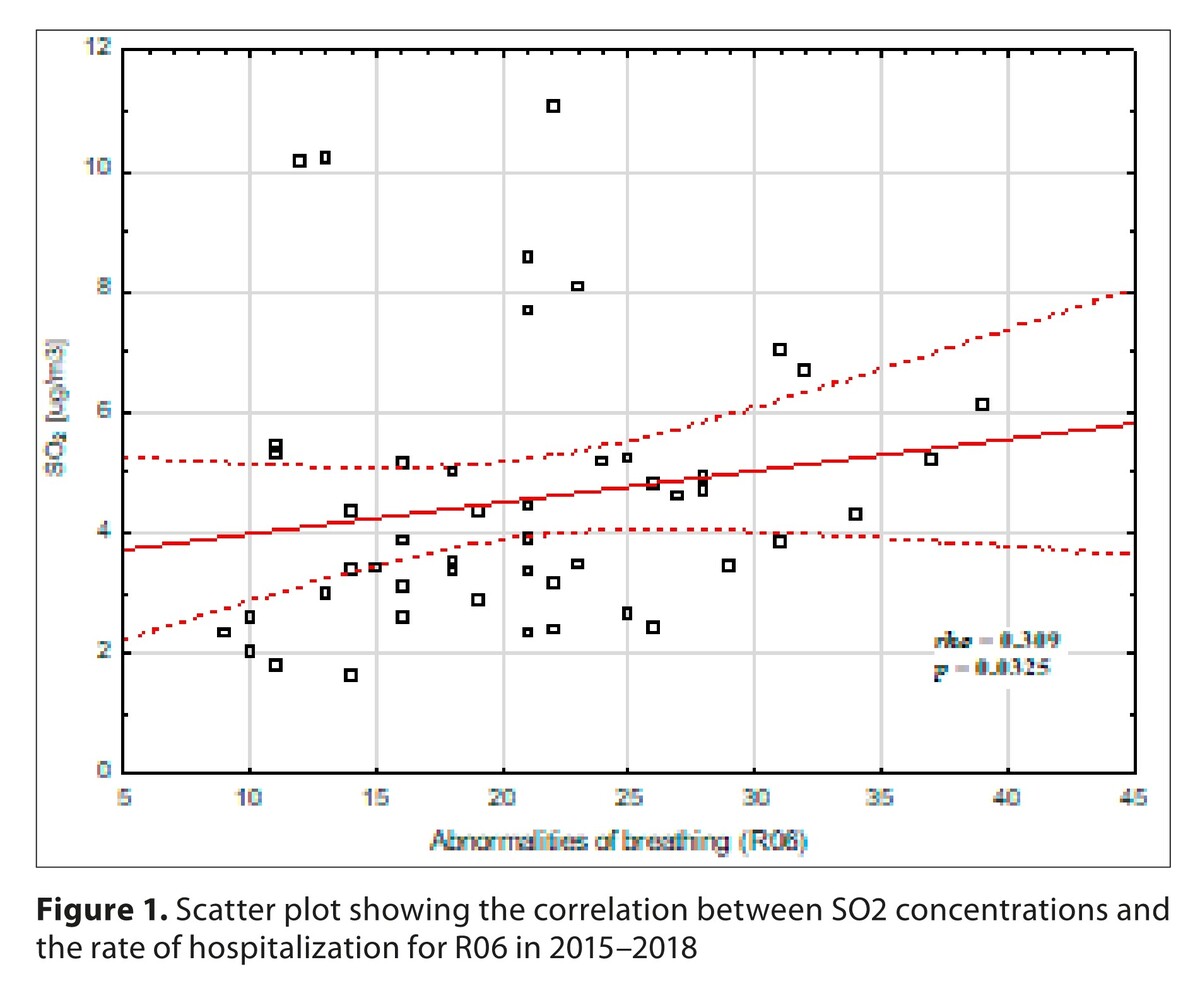
A number of statistically significant correlations were shown indicating the role of increased concentrations of each of the tested contaminants in the frequency of hospitalizations. In particular, strongly positive correlations were shown between the frequency of hospitalizations due to COPD and PM2.5 and PM10, asthma with benzene and NO2, and for respiratory disorders in general with benzene, CO and SO2.
Conclusions:
The results indicate that air pollution can be a significant modifiable risk factor for exacerbations of respiratory diseases and therefore its avoidance plays an important role in primary prevention.
Smog, which contains fine dusts, non-metal oxides, metals and organic compounds can have irritating, allergenic and immunomodulatory effects leading to the development of respiratory diseases and their exacerbations. The aim of the study was to search for a relationship between concentrations of air pollutants and the frequency of hospitalizations due to exacerbation of asthma, chronic obstructive pulmonary disease, or abnormalitis in breathing.
Material and methods:
Hospital admission data was accessed from the hospital digital in-formation system. From the publicly available database of the Chief Inspectorate for Environmental Protection, data concerning the concentrations of pollutants, such as PM2.5 and PM10, sulphur oxide IV (SO2), nitric oxide IV (NO2), carbon monoxide II (CO), benzene and ozone (O3), measured daily with hourly accuracy was used. The results of the average concentrations of air pollutants were compared with the rates of hospitalization in the corresponding time intervals.
Results:
A number of statistically significant correlations were shown indicating the role of increased concentrations of each of the tested contaminants in the frequency of hospitalizations. In particular, strongly positive correlations were shown between the frequency of hospitalizations due to COPD and PM2.5 and PM10, asthma with benzene and NO2, and for respiratory disorders in general with benzene, CO and SO2.
Conclusions:
The results indicate that air pollution can be a significant modifiable risk factor for exacerbations of respiratory diseases and therefore its avoidance plays an important role in primary prevention.
REFERENCES (54)
1.
Grzywa-Celińska A, Krusiński A, Milanowski J. ‘Smoging kills’ – Effects of air pollution on human respiratory system. Ann Agric Environ Med. 2020;27(1):1–5. https://doi.org/10.26444/aaem/....
2.
Szalontai K, Gémes N, Furák J, et al. Chronic obstructive pulmonary disease: epidemiology, biomarkers, and paving the way to lung cancer. J Clin Med. 2021;10(13):2889. https://doi.org/10.3390/jcm101....
3.
Dharmage SC, Perret JL, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7:246. https://doi.org/10.3389/fped.2....
4.
Hutchinson A, Pickering A, Williams P, et al. Breathlessness and presentation to the emergency department: a survey and clinical record review. BMC Pulm Med. 2017;17(1):53. https://doi.org/10.1186/s12890....
5.
Shrestha AP, Shrestha R, Shrestha SK, et al. Prevalence of dyspnea among patients attending the Emergency Department of a Tertiary Care Hospital: a descriptive cross-sectional study. J Nepal Med Assoc. 2019;57(219):302–306. https://doi.org/10.31729/jnma.....
6.
International Statistical Classification of Diseases and Related Health Problems 10th Revision, WHO. https://ICD-10 Version:2010 (who.int) (access: 2023.05.07).
7.
Madani NA, Carpenter DO. Patterns of emergency room visits for respiratory diseases in New York State in relation to air pollution, poverty and smoking. Int J Environ Res Public Health. 2023;20(4):3267. https://doi.org/10.3390/ijerph....
8.
Błaszczyk RT, Gorlo A, Dukacz M, et al. Association between exposure to air pollution and incidence of atrial fibrillation. Ann Agric Environ Med. 2023;30(1):15–21. https://doi.org/10.26444/aaem/....
9.
World Health Organization (2021). WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. World Health Organization. https://apps.who.int/iris/hand.... Licence: CC BY-NC-SA 3.0 IGO (access: 2023.05.07).
10.
DIRECTIVE 2008/50/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 21 May 2008 on ambient air quality and cleaner air for Europe EUR-Lex-32008L0050-EN-EUR-Lex (europa.eu) (access: 2023.05.07).
11.
Sahoo BM, Ravi Kumar BVV, Banik BK, et al. Polyaromatic hydro-carbons (PAHs): structures, synthesis and their biological profile. Curr Org Synth. 2020;17(8):625–640. https://doi.org/10.2174/157017....
12.
Von Burg R. Toxicology update: sulfur dioxide. J Appl Toxicol. 1996;16:365–371. https://doi.org/10.1002/(SICI)...<365:AID-JAT360>3.0.CO;2-H.
13.
Bahadar H, Mostafalou S, Abdollahi M. Current understandings and perspectives on non-cancer health effects of benzene: a global concern. Toxicol Appl Pharmacol. 2014;276(2):83–94. https://doi.org/10.1016/j.taap....
14.
Oftedal B, Nafstad P, Magnus P, et al. Traffic related air pollution and acute hospital admission for respiratory diseases in Drammen, Norway 1995–2000. Eur J Epidemiol. 2003;18(7):671–5. https://doi.org/10.1023/a:1024....
15.
Ran J, Sun S, Yang A, et al. Effects of ambient benzene and toluene on emergency COPD hospitalizations: A time series study in Hong Kong. Sci Total Environ. 2019;657:28–35. https://doi.org/10.1016/j.scit....
16.
Arif AA, Shah SM. Association between personal exposure to volatile organic compounds and asthma among the US adult population. Int Arch Occup Environ Health. 2007;80(8):711–9. Erratum in: Int Arch Occup Environ Health. 2008;81(4):503. https://doi.org/10.1007/s00420....
17.
Pénard-Morand C, Raherison C, Charpin D, et al. Long-term exposure to close-proximity air pollution and asthma and allergies in urban children. Eur Respir J. 2010;36(1):33–40. https://doi.org/10.1183/090319....
18.
Ko FWS, Tam W, Wong TW, et al. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong, Thorax. 2007;62:780–785. https://doi.org/10.1136/thx.20....
19.
Qibin L, Yacan L, Minli J, et al. The impact of PM2.5 on lung function in adults with asthma. Int J Tuberc Lung Dis. 2020;24(6):570–576. https://doi.org/10.5588/ijtld.....
20.
Vahedian M, Khanjani N, Mirzaee M, et al. Associations of short-term exposure to air pollution with respiratory hospital admissions in Arak, Iran. J Environ Health Sci Eng. 2017;15:17. https://doi.org/10.1186/s40201....
21.
Li Z, Lu F, Liu M, et al. Short-term effects of carbon monoxide on morbidity of chronic obstructive pulmonary disease with comorbidities in Beijing. Geohealth. 2023;7(3):e2022GH000734. https://doi.org/10.1029/2022GH....
22.
Kumar P, Singh AB, Arora T, et al. Critical review on emerging health effects associated with the indoor air quality and its sustainable management. Sci Total Environ. 2023;872:162163. https://doi.org/10.1016/j.scit....
23.
Evangelopoulos D, Chatzidiakou L, Walton H, et al. Personal exposure to air pollution and respiratory health of COPD patients in London. Eur Respir J. 2021;58(1):2003432. https://doi.org/10.1183/139930....
24.
Chang Q, Zhang H, Zhao Y. Ambient air pollution and daily hospital admissions for respiratory system-related diseases in a heavy polluted city in Northeast China. Environ Sci Pollut Res Int. 2020;27(9):10055–10064. https://doi.org/10.1007/s11356....
25.
Canova C, Torresan S, Simonato L, et al. Carbon monoxide pollution is associated with decreased lung function in asthmatic adults. Eur Respir J. 2010;35:266–272. https://doi.org/10.1183/090319....
26.
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383(9928):1581–92. https://doi.org/10.1016/S0140-....
27.
Chen CH, Wu CD, Lee YL, et al. Air pollution enhances the progression of restrictive lung function impairment and diffusion capacity reduction: an elderly cohort study. Respir Res. 2022;23(1):186. https://doi.org/10.1186/s12931....
28.
Saki H, Goudarzi G, Jalali S, et al. Study of relationship between nitrogen dioxide and chronic obstructive pulmonary disease in Bushehr, Iran. Clin Epid Glob Health. 2020;8(2):446–449. https://doi.org/10.1016/j.cegh....
29.
Zhang Z, Wang J, Lu W. Exposure to nitrogen dioxide and chronic obstructive pulmonary disease (COPD) in adults: a systematic review and meta-analysis. Environ Sci Pollut Res. 2018;25:15133–15145. https://doi.org/10.1007/s11356....
30.
Chan YL, Wang B, Chen H, et al. Pulmonary inflammation induced by low-dose particulate matter exposure in mice. Am J Physiol Lung Cell Mol Physiol. 2019;317(3):L424-L430. https://doi.org/10.1152/ajplun....
31.
Hoffmann C, Maglakelidze M, von Schneidemesser E, et al. Asthma and COPD exacerbation in relation to outdoor air pollution in the metropolitan area of Berlin, Germany. Respir Res. 2022;23(1):64. https://doi.org/10.1186/s12931....
32.
Lin CH, Wong LT, Hsu JY, et al. Relationship between exposure to ozone and exacerbation requiring hospital admission among patients with asthma: a case-control study in central Taiwan. BMJ Open. 2022;12(2):e050861. https://doi.org/10.1136/bmjope....
33.
Skowera B, Zuśka Z, Baranowska A. Temporal variability of tropospheric ozone pollution in the agricultural region of Central-Eastern Poland. Sustainability. 2020;12(18):7633. https://doi.org/10.3390/su1218....
34.
Avnery S, Mauzerall D, Liu J, et al. Global crop yield reductions due to surface ozone exposure: 1. Year 2000 crop production losses and economic damage. Atmos. Environ. 2011;45:2284–2296. https://doi.org/10.1016/j.atmo....
35.
Hazucha MJ, Bates DV, Bromberg PA. Mechanism of action of ozone on the human lung. J Appl Physiol. 1989;67(4):1535–41. https://doi.org/10.1152/jappl.....
36.
Paulin LM, Gassett AJ, Alexis NE, et al. Association of long-term ambient ozone exposure with respiratory morbidity in smokers. JAMA Intern Med. 2020;180(1):106–115. https://doi.org/10.1001/jamain....
37.
Kim SY, Kim E, Kim WJ. Health effects of ozone on respiratory diseases. Tuberc Respir Dis (Seoul). 2020;83:S6-S11. https://doi.org/10.4046/trd.20....
38.
Lin G, Wang Z, Zhang X, et al. Comparison of the association between different ozone indicators and daily respiratory hospitalization in Guangzhou, China. Front Public Health. 2023;11:1060714. https://doi.org/10.3389/fpubh.....
39.
Gao H, Wang K, Au WW, et al. A systematic review and meta-analysis of short-term ambient ozone exposure and COPD hospitalizations. Int J Environ Res Public Health. 2020;17:2130. https://doi.org/10.1002/jmv.26....
40.
Niewiadomska E, Kowalska M, Czech E. The risk of respiratory incidents in response to the increase of ozone concentration in the ambient air, in the Silesian Voivodeship, in 2016–2017. Przegl Epidemiol. 2022;76(2):216–229. https://doi.org/10.32394/pe.76....
41.
Jin L, Zhou T, Fang S, et al. Association of air pollutants and hospital admissions for respiratory diseases in Lanzhou, China, 2014–2019. Environ Geochem Health. 2022;6:1–19. https://doi.org/10.1007/s10653....
42.
Pedersen SE, Hurd SS, Lemanske RF Jr, et al. Global Initiative for Asthma. Global strategy for the diagnosis and management of asthma in children 5 years and younger. Pediatr Pulmonol. 2011;46(1):1–17. https://10.1002/ppul.21321.
43.
Nurhisanah S, Hasyim H. Environmental health risk assessment of sulfur dioxide (SO2) at workers around in combined cycle power plant (CCPP). Heliyon. 2022;8(5):e09388. https://doi.org/10.1016/j.heli....
44.
Lin AH, Hsu CC, Lin YS, et al. Mechanisms underlying the stimulatory effect of inhaled sulfur dioxide on vagal bronchopulmonary C-fibres. J Physiol. 2020;598(5):1093–1108. https://doi.org/10.1113/JP2791....
45.
Zhou X, Gao Y, Wang D, et al. Association between sulfur dioxide and daily inpatient visits with respiratory diseases in Ganzhou, China: a time series study based on hospital data. Front Public Health. 2022;10:854922. https://doi.org/10.3389/fpubh.....
46.
Tomić-Spirić V, Kovačević G, Marinković J, et al. Sulfur dioxide and exacerbation of allergic respiratory diseases: A time-stratified case-crossover study. J Res Med Sci. 2021;26:109. https://doi.org/10.4103/jrms.J....
47.
Cheng CG, Yen SY, Hsiao CC, et al. Short-term exposure effect of ambient fine particulate matter, ozone and cold temperature on emergency room visits for asthma patients. Toxics. 2023;11(2):94. https://doi.org/10.3390/toxics....
48.
Zhao Y, Hu J, Tan Z, et al. Ambient carbon monoxide and increased risk of daily hospital outpatient visits for respiratory diseases in Dongguan, China. Sci Total Environ. 2019;668:254–260. https://doi.org/10.1016/j.scit....
49.
Rzymski P, Poniedziałek B, Rosińska J, et al. Air pollution might affect the clinical course of COVID-19 in pediatric patients. Ecotoxicol Environ Saf. 2022;239:113651. https://doi.org/10.1016/j.ecoe....
50.
Gangadi M, Dounias G, Bakakos P, et al. Air pollution and hospital admission for respiratory diseases in Athens, Greece. Eur Resp J. 2019;54:PA2841. https://doi.org/10.1183/139930....
51.
Slaughter JC, Kim E, Sheppard L, et al. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Expo Sci Environ Epidemiol. 2005;15(2):153–159. https://doi.org/10.1038/sj.jea....
53.
Wielgosiński G, Czerwińska, J. Smog Episodes in Poland. Atmosphere. 2020;11:277. https://doi.org/10.3390/atmos1....
54.
Szyszkowicz M, Kousha T, Castner J, et al. Air pollution and emergency department visits for respiratory diseases: A multicity case crossover study. Environ Res. 2018;163:263–269. https://doi.org/10.1016/j.envr....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.