Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
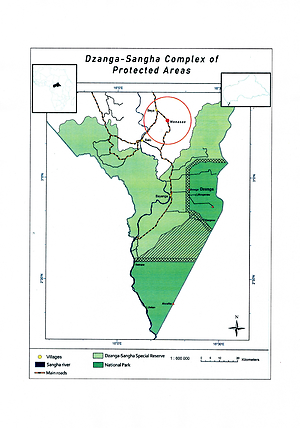
Prevalence of Plasmodium spp. in symptomatic BaAka Pygmies inhabiting the rural Dzanga Sangha region of the Central African Republic
1
4th Department of Infectious Diseases, Provincial Hospital for Infectious Diseases, Warsaw, Poland
2
Military Institute of Medicine, Warsaw, Poland
3
Department of Tropical Parasitology, Institute of Maritime and Tropical Medicine, Medical University, Gdańsk, Poland
Corresponding author
Ann Agric Environ Med. 2021;28(3):483-490
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Malaria remains a diagnostic and therapeutic challenge in many endemic regions of sub-Saharan Africa. It is one of the most important causes of morbidity and mortality, especially in children <5 years. Plasmodium falciparum is responsible for the majority of severe malaria cases in sub-Saharan Africa, but is not the exclusive one.
Objective:
The objective of the study was to assess the prevalence of Plasmodium spp. in BaAka Pygmies with clinical symptoms of malaria, and define the percentage distribution of infections caused by species other than P. falciparum in order to assess the need for diversification of malaria treatment protocols.
Material and methods:
The study was conducted during the dry and rainy seasons in 2018 and involved a group of 540 symptomatic BaAka Pygmies, patients of both genders, aged 1–75-years-old. Two diagnostic methods for detecting Plasmodium in the bloodstream were used: RDTs targeting HRP2-protein specific for P. falciparum, and PCR assays aimed at detecting P. falciparum, P. vivax, P. ovale, P. malariae species.
Results:
Only 40.5% of symptomatic patients tested with RDTs for P. falciparum infections were positive. Molecular tests (PCR) confirmed P. falciparum in 94.8% of the samples and also revealed the genetic material of P. malariae (11.1%), P. ovale (9.8%), and P. vivax (0.7%). BaAka Pygmies aged <5 years of age dominated in patients with positive results; the common clinical symptoms reported by the sick individuals were fever, shivers and fatigue.
Conclusions:
The study suggests the need for introducing accurate diagnostic methods for the diagnosis of malaria and the revision of malaria treatment protocols. Assessment of the Pfhrp2/Pfhrp3 deletions is necessary for evaluating malaria epidemiology in Central Africa.
Malaria remains a diagnostic and therapeutic challenge in many endemic regions of sub-Saharan Africa. It is one of the most important causes of morbidity and mortality, especially in children <5 years. Plasmodium falciparum is responsible for the majority of severe malaria cases in sub-Saharan Africa, but is not the exclusive one.
Objective:
The objective of the study was to assess the prevalence of Plasmodium spp. in BaAka Pygmies with clinical symptoms of malaria, and define the percentage distribution of infections caused by species other than P. falciparum in order to assess the need for diversification of malaria treatment protocols.
Material and methods:
The study was conducted during the dry and rainy seasons in 2018 and involved a group of 540 symptomatic BaAka Pygmies, patients of both genders, aged 1–75-years-old. Two diagnostic methods for detecting Plasmodium in the bloodstream were used: RDTs targeting HRP2-protein specific for P. falciparum, and PCR assays aimed at detecting P. falciparum, P. vivax, P. ovale, P. malariae species.
Results:
Only 40.5% of symptomatic patients tested with RDTs for P. falciparum infections were positive. Molecular tests (PCR) confirmed P. falciparum in 94.8% of the samples and also revealed the genetic material of P. malariae (11.1%), P. ovale (9.8%), and P. vivax (0.7%). BaAka Pygmies aged <5 years of age dominated in patients with positive results; the common clinical symptoms reported by the sick individuals were fever, shivers and fatigue.
Conclusions:
The study suggests the need for introducing accurate diagnostic methods for the diagnosis of malaria and the revision of malaria treatment protocols. Assessment of the Pfhrp2/Pfhrp3 deletions is necessary for evaluating malaria epidemiology in Central Africa.
ABBREVIATIONS
CAR – Central African Republic; WHO – World Health Organization; PCR – polymerase chain reaction; RDT – rapid diagnostic test; HRP2 – histidine rich protein 2; ACT – artemisinin-combined therapy; NGO – non–governmental organization; FUO – fever of unknown origin
ACKNOWLEDGEMENTS
The authors would like to thank Emmanuel Wane, director of the ADIH Hospital in Bayanga for assistance obtaining agreement for the research from the Ministry of Research and Innovative Technologies in the Central African Republic.
The research received financial support from Ministry of Science and Higher Education in Warsaw, Poland (Grant No. 556/2018). The ministry had no role in study design, collection and analyse of data, decision to publish, or preparation of the manuscript.
The study entitled Assessment of the prevalence Plasmodium infections in sub-Saharan Africa in symptomatic BaAka Pygmies inhabiting the rural Dzanga Sangha region in the Central African Republic was approved by the Bioethics
Committee at the Military Institute of Medicine, Warsaw, Poland (Resolution No. 137/WIM/2018).
The study entitled Evaluation de la survenue d’infections à Plasmodium spp dans la population de Pygmées BaAka des zones forestières de la République Centrafricaine was approved by the Ministry of Research and Innovative Technologies, Bangui, Central African Republic (Resolution No. 176/
MERSIT/DIRCAB/CB.18).
REFERENCES (42)
1.
World Health Organization. World Malaria Report 2019. https://www.who.int/publicatio... item/world-malaria-report-2019 (access: 2020.09.22).
2.
Centers for Disease Control and Prevention. Malaria‘s Impact Worldwide. https://www.cdc.gov/ malaria/malaria_worldwide/impact.html (access: 2020.09.20).
3.
World Health Organization. Central African Republic. https://www.who.int/malaria/ publications/country-profiles/profile_caf_en.pdf?ua=1 (access: 2020.10.07).
4.
World Health Organization. Malaria Rapid Diagnostic Test Performance. Results of WHO product testing of malaria RDTs: round 8 (2016–2018). Geneva: WHO; 2018. (access: 2020.07.28).
5.
World Health Organization. https://www.who.int/hac/crises... lic_country_fact_sheet_march2014.pdf (access: 2021.02.06).
8.
Mangham LJ, Cundill B, Achonduh OA, et al. Malaria prevalence and treatment of febrile patients at health facilities and medicine retailers in Cameroon. Trop Med Int Health. 2012; 17(3): 330–342. https://doi.org/10.1111/j.1365....
9.
Rapport de suivi des 100 indicateurs clés en 2019. http://onsp.minsante.cm/sites/... publications/217/ Rapport de suivi des 100 indicateurs clés en 2019.pdf (access: 2020.11.08).
10.
Antonio-Nkondjio, C, Ndo C, Njiokou F, et al. Review of malaria situation in Cameroon: technical viewpoint on challenges and prospects for disease elimination. Parasit Vectors. 2019; 12(1): 501. https://doi.org/10.1186/s13071....
11.
Fru-Cho J, Bumah VV, Safeukui I, et al. Molecular typing reveals substantial Plasmodium vivax infection in asymptomatic adults in a rural area of Cameroon. Malar J. 2014; 13: 170. https://doi.org/10.1186/1475-2....
12.
Russo G, Faggioni G, Paganotti G, et al. Molecular evidence of Plasmodium vivax infection in Duffy negative symptomatic individuals from Dschang, West Cameroon. Malaria J. 2017; 16(1): 74. https://doi.org/10.1186/s12936....
13.
Ndo C, Kopya E, Donbou MA, et al. Elevated Plasmodium infection rates and high pyrethroid resistance in major malaria vectors in a forested area of Cameroon highlight challenges of malaria control. Parasit Vectors. 2018; 11(1): 157. https://doi.org/10.1186/s13071....
14.
Tabue RN, Njeambosay BA, Zeukeng F, et al. Case Definitions of Clinical Malaria in Children from Three Health Districts in the North Region of Cameroon. Biomed Res Int. 2019; 2019: 9709013. https://doi.org/10.1155/2019/9....
15.
Tsumori Y, Ndounga M, Sunahara T, et al. Plasmodium falciparum: differential selection of drug resistance alleles in contiguous urban and peri-urban areas of Brazzaville, Republic of Congo. PLoS One. 2011; 6(8): e23430. https://doi.org/10.1371/journa....
16.
Koukouikila-Koussounda F, Ntoumi F. Malaria epidemiological research in the Republic of Congo. Malaria J. 2016; 15(1): 598. https://doi.org/10.1186/s12936....
17.
Ntoumi F, Vouvoungui J, Ibara R, et al. Malaria burden and case management in the Republic of Congo: limited use and application of rapid diagnostic tests results. BMC Public Health. 2013; 13(1): 135. https://doi.org/10.1186/1471-2....
18.
Koukouikila-Koussounda F, Malonga V, Mayengue PI, et al. Genetic polymorphism of merozoite surface protein 2 and prevalence of K76T pfcrt mutation in Plasmodium falciparum field isolates from Congolese children with asymptomatic infections. Malar J. 2012; 11: 105. https://doi.org/10.1186/1475-2....
19.
Culleton R, Ndounga M, Zeyrek FY, et al. Evidence for the transmission of Plasmodium vivax in the Republic of the Congo, West Central Africa. J Infect Dis. 2009; 200(9): 1465–1469. https://doi.org/10.1086/644510.
20.
Roucher C, Rogier C, Sokhna C, et al. A 20-year longitudinal study of Plasmodium ovale and Plasmodium malariae prevalence and morbidity in a West African population. PLoS One. 2014; 9(2): e87169. https://doi.org/10.1371/journa....
21.
World Health Organization. Guidelines for the treatment of malaria. 3rd edition. Geneva: WHO; 2015 (access: 2020.10.20).
22.
Chandler C, Jones C, Boniface G, et al. Guidelines and mindlines: why do clinical staff over-diagnose malaria in Tanzania? A qualitative study. Malaria J. 2008; 7(1): 53. https://doi.org/10.1186/1475-2....
23.
Omitola O, Mogaji H, Taylor-Robinson A. Managing Febrile Illness in Malaria-endemic Areas: Developing Novel Diagnostics Using Host Immunological Signatures as Surrogate Markers of Infection. Curr Immunol Rev. 2019; 15(2): 202–206. https://doi.org/10.2174/157339....
24.
Tadesse BT, Ashley EA, Ongarello S, et al. Antimicrobial resistance in Africa: a systematic review. BMC Infect Dis. 2017; 17(1): 616. https://doi.org/10.1186/s12879....
25.
Djallé D, Gody JC, Moyen JM, et al. Performance of Paracheck™-Pf, SD Bioline malaria Ag-Pf and SD Bioline malaria Ag-Pf/pan for diagnosis of falciparum malaria in the Central African Republic. BMC Infect Dis. 2014; 14: 109. https://doi.org/10.1186/1471-2....
26.
Dollat M, Talla C, Sokhna C, et al. Measuring malaria morbidity in an area of seasonal transmission: Pyrogenic parasitemia thresholds based on a 20-year follow-up study. PLoS One. 2019; 14(6): e0217903. https://doi.org/10.1371/journa....
27.
Cohen S, McGregor IA, Carrington S. Gamma-globulin and acquired immunity to human malaria. Nature. 1961; 192: 733–737. https://doi.org/10.1038/192733....
28.
Kurtovic L, Boyle MJ, Opi DH, et al. Complement in malaria immunity and vaccines. Immunol Rev. 2020; 293(1): 38–56. https://doi.org/10.1111/imr.12....
29.
Proietti C, Krause L, Trieu A, et al. Immune Signature Against Plasmodium falciparum Antigens Predicts Clinical Immunity in Distinct Malaria Endemic Communities. Mol Cell Proteomics. 2020; 19(1): 101–113. https://doi.org/10.1074/mcp.RA....
30.
Chen I, Clarke SE, Gosling R, et al. “Asymptomatic” Malaria: A Chronic and Debilitating Infection That Should Be Treated. PLoS Med. 2016; 13(1): e1001942. https://doi.org/10.1371/journa....
31.
Gendrot M, Fawaz R, Dormoi J, et al. Genetic diversity and deletion of Plasmodium falciparum histidine-rich protein 2 and 3: a threat to diagnosis of P. falciparum malaria. Clin Microbiol Infect. 2019; 25(5): 580–585. https://doi.org/10.1016/j.cmi.....
32.
Trouvay M, Palazon G, Berger F, et al. High performance of histidine-rich protein 2 based rapid diagnostic tests in French Guiana are explained by the absence of pfhrp2 gene deletion in P. falciparum. PLoS One. 2013; 8(9): e74269. https://doi.org/10.1371/journa....
33.
Baker J, Ho MF, Pelecanos A, et al. Global sequence variation in the histidine-rich proteins 2 and 3 of Plasmodium falciparum: implications for the performance of malaria rapid diagnostic tests. Malar J. 2010; 9: 129. https://doi.org/10.1186/1475-2....
34.
Nyataya J, Waitumbi J, Mobegi V, et al. Plasmodium falciparum Histidine-Rich Protein 2 and 3 Gene Deletions and Their Implications in Malaria Control. Diseases. 2020; 8(2): 15. https://doi.org/10.3390/diseas....
35.
Gamboa D, Ho MF, Bendezu J, et al. A large proportion of P. falciparum isolates in the Amazon region of Peru lack pfhrp2 and pfhrp3: implications for malaria rapid diagnostic tests. PLoS One. 2010; 5(1): e8091. https://doi.org/10.1371/journa.... pone.0008091.
36.
Berhane A, Anderson K, Mihreteab S, et al. Major Threat to Malaria Control Programs by Plasmodium falciparum Lacking Histidine-Rich Protein 2, Eritrea. Emerg Infect Dis. 2018; 24(3): 462–470. https://doi.org/10.3201/eid240....
37.
Agaba BB, Yeka A, Nsobya S, et al. Systematic review of the status of pfhrp2 and pfhrp3 gene deletion, approaches and methods used for its estimation and reporting in Plasmodium falciparum populations in Africa: review of published studies 2010–2019. Malar J. 2019; 18(1): 355. https://doi.org/10.1186/s12936....
38.
World Health Organization. Protocol for estimating the prevalence of pfhrp2/pfhrp3gene deletions among symptomatic falciparum patients with false-negative RDT results. Geneva: WHO; 2018 (access: 2020.10.20).
39.
Parr JB, Verity R, Doctor SM, et al. Pfhrp2-Deleted Plasmodium falciparum Parasites in the Democratic Republic of the Congo: A National Cross-sectional Survey. J Infect Dis. 2017; 216(1): 36–44. https://doi.org/10.1093/infdis....
40.
Markwalter CF, Mudenda L, Leelawong M, et al. Evidence for histidine-rich protein 2 immune complex formation in symptomatic patients in Southern Zambia. Malar J. 2018; 17(1): 256. https://doi.org/10.1186/s12936....
41.
Dalrymple U, Arambepola R, Gething PW, et al. How long do rapid diagnostic tests remain positive after anti-malarial treatment? Malar J. 2018; 17(1): 228. https://doi.org/10.1186/s12936....
42.
World Health Organization. Universal access to malaria diagnostic testing – an operational manual. Geneva: WHO; 2013. http://www.who.int/malaria/pub... en/ (access: 2020.07.28).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.