Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Intestinal parasitic infections in a population of BaAka Pygmies inhabiting the Congo Basin in the Central African Republic
1
Military Institute of Medicine, Warsaw, Poland
2
Medical University, Gdańsk, Poland
3
Provincial Hospital for Infectious Diseases, Warsaw, Poland
4
Medical University, Wrocław, Poland
Corresponding author
Ann Agric Environ Med. 2021;28(1):127-130
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Pygmy tribes inhabit tropical environment of Central Africa. After expulsion from their original habitat by the Bantu people, they settled in a local forest ecosystem where they live with very low sanitary standards. Their actual morbidity remains unknown.
Objective:
The aim of the study was to analyze the prevalence of intestinal parasitic infections in BaAka Pygmies inhabiting the Congo Basin in the Central African Republic.
Material and methods:
The study was conducted in 2015, and involved a group of 950 Pygmies living inthe Sangha-Mbaere and Lobaye prefectures. Single stool samples were collected from study participants, fixed in 10% formalin, transported from Africa to Europe, and analyzed by light microscopy using 5 different diagnostic methods (direct smear, decantation with distilled water, Fülleborne’s flotation, Kato-Miura thick smear, DiaSyS/PARASYS system sedimentation) at the Military Institute of Medicine in Warsaw, Poland.
Results:
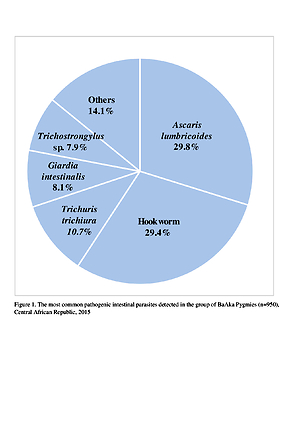
Microscopic examination revealed infections with 14 different species of intestinal nematodes, cestodes, trematodes and protozoa. According to the study findings, 90.5% of BaAka Pygmies were found to be infected with intestinal parasites, and 70.8% had mixed infections. Most of the pathogenic intestinal parasites were nematodes (85.0%), with Asrcaris lumbricoides (29.8%), hookworm (29.4%) and Trichuris trichiura (10.7%) being predominant.
Conclusions:
Poor sanitation, limited the high prevalence of intestinal parasitic infections in the community of Pygmies. The negative test results may prove the effectiveness of periodic deworming campaigns chich, implemented by non-governmental organizations, are voluntary with respect to the informed consent principle.
Pygmy tribes inhabit tropical environment of Central Africa. After expulsion from their original habitat by the Bantu people, they settled in a local forest ecosystem where they live with very low sanitary standards. Their actual morbidity remains unknown.
Objective:
The aim of the study was to analyze the prevalence of intestinal parasitic infections in BaAka Pygmies inhabiting the Congo Basin in the Central African Republic.
Material and methods:
The study was conducted in 2015, and involved a group of 950 Pygmies living inthe Sangha-Mbaere and Lobaye prefectures. Single stool samples were collected from study participants, fixed in 10% formalin, transported from Africa to Europe, and analyzed by light microscopy using 5 different diagnostic methods (direct smear, decantation with distilled water, Fülleborne’s flotation, Kato-Miura thick smear, DiaSyS/PARASYS system sedimentation) at the Military Institute of Medicine in Warsaw, Poland.
Results:
Microscopic examination revealed infections with 14 different species of intestinal nematodes, cestodes, trematodes and protozoa. According to the study findings, 90.5% of BaAka Pygmies were found to be infected with intestinal parasites, and 70.8% had mixed infections. Most of the pathogenic intestinal parasites were nematodes (85.0%), with Asrcaris lumbricoides (29.8%), hookworm (29.4%) and Trichuris trichiura (10.7%) being predominant.
Conclusions:
Poor sanitation, limited the high prevalence of intestinal parasitic infections in the community of Pygmies. The negative test results may prove the effectiveness of periodic deworming campaigns chich, implemented by non-governmental organizations, are voluntary with respect to the informed consent principle.
REFERENCES (23)
1.
Chacin-Bonilla L. Intestinal parasitic diseases as a global health problem. Invest Clin. 2013; 54(1): 1–4.
2.
World Health Organization. Intestinal worms. Epidemiology, geographical distribution. Available at: https://www.who.int/intestinal... (access: 2020.10.01).
3.
Karagiannis-Volues DA, Biedermann P, Ekpo UF, Garba A, Langner E, Mathieu E, et al. Spatial and temporal distribution of soil-transmitted helminth infection in sub-Saharan Africa: a systemic review and geostatistical meta-analysis. Lancet Infect Dis. 2015; 15(1): 74–84.
4.
Diggle PJ, Giorgi E. Geostatistical mapping of helminth infection rates. Lancet Infect. Dis. 2015; 15(1): 9–11.
5.
Korzeniewski K, Lass A, Augustynowicz A, Konior M. The Prevalence of Intestinal Parasitic Infections Among Kosovar and Serbian School-children in Kosovo. Helminthologia. 2020; 57(3): 276–279.
6.
El-Sherbini GT, Abosdera MM. Risk factors associated with intestinal parasitic infections among children. J Egypt Soc Parasitol. 2013; 43: 287–294.
7.
Jourdan PM, Lamberton PH, Fenwick A, Addiss DG. Soil-transmitted helminth infections. Lancet. 2018; 391(10117): 252–265.
8.
The United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Central African Republic – situation report 23 Oct 2020. Available at: https://reliefweb.int/sites/re... (access: 2020.10.26).
9.
Hewlett BS. (Ed.). Hunter-Gatherers of the Congo Basin; Cultures, Histories and Biology of African Pygmies. Transaction Publishers: New Brunswick and London 2014.
10.
Garcia LS. Practical Guide to Diagnostic Parasitology. 2nd Ed. ASM Press: Washington DC, USA 2009.
11.
Kettelhut M, Moody A, Edwards H, Chiodini PL. Evaluation of Parasep® Faecal Parasite Concentrator. Hospital for Tropical Diseases, London, England. 2003.06.07. Available at: https://journals.plos.org/plos...= info:doi/10.1371/journal.pntd.0000386.s002 (access: 2020.10.01).
12.
Friesen J, Bergman C, Neuber R, Fuhrmann J, Wenzel T, Durst A, et al. Detection of Enterobius vermicularis in greater Berlin, 2007–2017: seasonality and increased frequency of detection. Eur J Clin Microbiol Infect Dis. 2019; 38(4): 719–723.
13.
Reh L, Muadica AS, Köster PC, Balasegaram S, Verlander NQ, Chercoles ER, et al. Substancial prevalence of enteroparasites Cryptosporidium spp., Giardia duodenalis and Blastocystis sp. in asymptomatic schoolchildren in Madrid, Spain, November 2017 to June 2018. Euro Surveill. 2019; 24(43): 1900241.
14.
Mamo H. Intestinal Parasitic Infections among Prison Inmates and Tobacco Farm Workers in Shewa Robit, North Central Ethiopia. PLoS One. 2014; 9(6): e99559.
15.
Vouking MZ, Enoka P, Tamo CV, Tandefok CN. Prevalence of intestinal parasites among HIV patients at the Yaound Central Hospital, Cameroon. Pan Afr Med J. 2014; 18: 136.
16.
Tefera T, Mebrie G. Prevalence and Predictors of Intestinal Parasites among Food Handlers in Yebu Town, Southwest Ethiopia. PLoS One. 2014; 9(10): e110621.
17.
Shiferaw MB, Mengistu AD. Helminthiasis: Hookworm Infection Remains a Public Health Problem in Dera District, South Gondar, Ethiopia. PLoS One. 2015; 10(12): e0144588.
18.
Meunier DM, Georges MC, Georges AJ. Report on intestinal parasitosis in adults in an urban population of the Central African Republic. Bull Soc Pathol Exot Filiales. 1984; 77(3): 333–343.
19.
Tekpa G, Fikouma V, Gbangba-Ngai E, Bogning Mejiozem BO, Ningatouloum Nazita, S, Koffi B. Epidemiological and clinical profile of intestinal parasitosis of children in rural areas in Central African Republic. Arch Pediatr. 2019; 26: 34–37.
20.
Meurs L, Polderman AM, Vinkeles Melchers NV, Brienen EA, Verweij JJ, et al. Diagnosing Polyparasitism in a High-Prevalence Setting in Beira, Mozambique: Detection of Intestinal Parasites in Fecal Samples by Microscopy and Real-Time PCR. PLoS Negl Trop Dis. 2017; 11(1): e0005310.
21.
Engels D. (Ed.). Preventive chemotherapy in human helminthiasis. Coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. Geneva: WHO/Department of Control of Neglected Tropical Diseases 2006. Available at: https://www.who.int/neglected_... (access: 2020.10.09).
22.
Truscott JE, Turner HC, Farrell SH, Anderson RM. Soil-Transmitted Helminths: Mathematical Models of Transmission, the Impact of Mass Drug Administration and Transmission Elimination Criteria. Adv Parasitol. 2016; 94: 133–198.
23.
Anderson RM, Turner HC, Farrell SH, Truscott JE. Studies of the Transmission Dynamics, Mathematical Model Development and the Control of Schistosome Parasites by Mass Drug Administration in Human Communities. Adv Parasitol. 2016; 94: 199–246.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.