Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Outcome of transobturator sling for treatment of female stress urinary incontinence applied as
a single procedure or concomitantly with pelvic organ prolapse surgery
1
2nd Department of Gynaecology, Medical University, Lublin, Poland
Corresponding author
Katarzyna Jankiewicz
II-nd Department of Gynecology, Medical University of Lublin, Jaczewskiego 8, 20-097, Lublin, Poland
II-nd Department of Gynecology, Medical University of Lublin, Jaczewskiego 8, 20-097, Lublin, Poland
Ann Agric Environ Med. 2023;30(1):190-194
KEYWORDS
Sub-urethral slingpelvic organ prolapsestress urinary incontinencetransobturator tapesling efficacyurine retention
TOPICS
ABSTRACT
Introduction and objective:
The aim of the study was to check the safety and efficacy of transobturator tape (TOT) combined with various prolapse procedures. The results were compared with outcomes of sling performed as an alone surgery. Risk factors for TOT failure were also identified.
Material and methods:
The study comprised 219 patients with sling alone (Group SUI) and 221 after TOT combined with concomitant prolapse surgery (Group POP/SUI). Medical records were carefully reviewed to obtain demographic and clinical data, details of surgery, including intra-and postoperative complications.
Results:
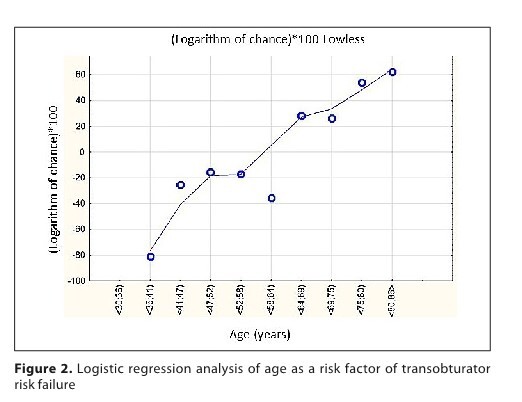
Subjective cure rate was slightly, but statistically significantly, higher in POP/SUI group (89.6% vs 82.6%; ch2 = 4.44; p = 0.035). There was no significant difference in sling efficacy dependant of type of POP surgery. Post-operative urine retention was more frequent in POP/SUI group compared to SUI group (18.6% vs 3.2%; ch2 = 34.36; p < 0.001). Logistic regression showed that age, BMI and prolonged pos-operative urine retention are independent factors affecting TOT outcome. Age ≥65years and BMI ≥30kg,m2 more than doubled the risk of failure: OR 2.348, CI 95% (1.330–4.147); p = 0.003 and 2.030, (95% CI 1.148–3.587); p = 0.015; respectively. Interestingly, post-operative urine retention appeared to be a positive prognostic factor OR 0.145, (95% CI 0.019–1.097); p < 0.05.
Conclusions:
Subjective efficacy of TOT used concomitantly with POP procedures is slightly higher than TOT alone. Better sling outcomes can be expected both for POP procedures involving both the anterior and posterior compartments. Age and obesity are independent factors of TOT failure, whereas prolonged post-operative urine retention is a positive predictive factor of TOT success.
The aim of the study was to check the safety and efficacy of transobturator tape (TOT) combined with various prolapse procedures. The results were compared with outcomes of sling performed as an alone surgery. Risk factors for TOT failure were also identified.
Material and methods:
The study comprised 219 patients with sling alone (Group SUI) and 221 after TOT combined with concomitant prolapse surgery (Group POP/SUI). Medical records were carefully reviewed to obtain demographic and clinical data, details of surgery, including intra-and postoperative complications.
Results:
Subjective cure rate was slightly, but statistically significantly, higher in POP/SUI group (89.6% vs 82.6%; ch2 = 4.44; p = 0.035). There was no significant difference in sling efficacy dependant of type of POP surgery. Post-operative urine retention was more frequent in POP/SUI group compared to SUI group (18.6% vs 3.2%; ch2 = 34.36; p < 0.001). Logistic regression showed that age, BMI and prolonged pos-operative urine retention are independent factors affecting TOT outcome. Age ≥65years and BMI ≥30kg,m2 more than doubled the risk of failure: OR 2.348, CI 95% (1.330–4.147); p = 0.003 and 2.030, (95% CI 1.148–3.587); p = 0.015; respectively. Interestingly, post-operative urine retention appeared to be a positive prognostic factor OR 0.145, (95% CI 0.019–1.097); p < 0.05.
Conclusions:
Subjective efficacy of TOT used concomitantly with POP procedures is slightly higher than TOT alone. Better sling outcomes can be expected both for POP procedures involving both the anterior and posterior compartments. Age and obesity are independent factors of TOT failure, whereas prolonged post-operative urine retention is a positive predictive factor of TOT success.
REFERENCES (38)
1.
Rubilotta E, Balzarro M, D’Amico A, et al. Pure stress urinary incontinence: analysis of prevalence, estimation of costs, and financial impact. BMC Urol. 2019;19(1):44. https://doi.org/10.1186/s12894....
2.
Hakimi S, Aminian E, Mohammadi M, et al. Prevalence and Risk Factors of Urinary/Anal Incontinence and Pelvic Organ Prolapse in Healthy Middle-Aged Iranian Women. J Menopausal Med. 2020;26(1):24–28. https://doi.org/10.6118/jmm.19....
3.
Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–1316. https://doi.org/10.1001/jama.3....
4.
Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;30(4):CD004014. https://doi.org/10.1002/146518....
5.
Bai SW, Leon MJ, Kim JY, et al. Relationship between stress urinary incontinence and pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(4):256–260. https://doi.org/10.1007/s00192....
6.
Rodríguez-Mias NL, Martinez-Franco EM, Aguado J, et al. Pelvic organ prolapse and stress urinary incontinence, do they share the same risk factors? Eur J Obstet Gynecol Reprod Biol. 2015;190:52–57. https://doi.org/10.1016/j.ejog....
7.
Vergeldt TFM, Weemhoff M, IntHout J, et al. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26(11):1559–1573. https://doi.org/10.1007/s00192....
8.
Dicpinigaitis PV. Prevalence of stress urinary incontinence in women presenting for evaluation of chronic cough. ERJ Open Res. 2021;7(1):00012–2021. https://openres.ersjournals.co....
9.
Allen-Brady K, Cannon-Albright LA, Farnham JM, et al. Evidence for pelvic organ prolapse predisposition genes on chromosomes 10 and 17. Am J Obstet Gynecol. 2015;212(6):771.e1–7. https://doi.org/10.1016/j.ajog....
10.
Burkhard FC, Bosch JLHR, Cruz F, et al. EAU Guidelines Office, Arnhem, 2022. The Netherlands. Online: http://uroweb.org/guidelines/c... [01.09.2020].
11.
National Institute for Health Care and Excellence. Urinary incontinence and pelvic organ prolapse: management 2019. Online: https://www.nice.org.uk/guidan... [01.09.2020].
12.
Baessler K, Christmann-Schmid C, Maher C, et al. Surgery for women with pelvic organ prolapse with or without stress urinary incontinence. Cochrane Database Syst Rev. 2018;8(8):CD013108. https://doi.org/10.1002/146518....
13.
Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(96):10–17. https://doi.org/10.1016/S0002-....
14.
Rechberger T, Futyma K, Jankiewicz K, et al. Tape Fixation: An Important Surgical Step to Improve Success Rate of Anti-Incontinence Surgery. The J Urol. 2010;18(1)6:180–84. https://doi.org/10.1016/j.juro....
15.
Skorupska K, Futyma K, Bogusiewicz M, et al. Four-arm polypropylene mesh for vaginal voult prolapse – surgical technicques and outcomes. Eur J Obstet Gynecol Reprod Biol. 2020;255:203–210. https://doi.org/10.1016/j.ejog....
16.
Skorupska K, Miotła P, Kubik-Komar A, et al. Development and validation of Polish version of the Urogenital Distress Inventory short form anf the Incontinence Impact Questionnaire short form. Eur J Obstet Gynecol Reprod Biol. 2017;215:171–174. https://doi.org/10.1016/j.ejog....
17.
Balzarro M, Rubilotta E, Trabacchin N, et al. A prospective comparative study of the feasibility and reliability of telephone follow-up in female urology: the patient home office novel evaluation (PHONE) study. Urology. 2020;136:82–87. https://doi.org/10.1016/j.urol....
18.
Chai TC, Kenton K, Xu Y, et al. Effects of concomitant surgeries during midurethral slings (MUS) on postoperative complications, voiding dysfunction, continence outcomes, and urodynamic variables. Urology. 2012;79(6):1256–1261. https://doi.org/10.1016/j.urol....
19.
Lo TS, Tan YL, Cortes EF et al. Influence of anterior vaginal mesh with concomitant mid-urethral sling surgery on stress urinary incontinence: clinical and sonographic outcome. Aust N Z J Obstet Gynaecol. 2015;55(6):593–600. https://doi.org/10.1111/ajo.12....
20.
Celik F, Pektas MK, Kose M et al. Two-Year Follow-Up Results of Transobturator Tape Procedure with and without Concomitant Vaginal Surgery. Urol Int. 2018;100(4):402–408. https://doi.org/10.1159/000488....
21.
Çoşkun B, Aksakal O, Çoşkun B et al. The impact of concurrent pelvic organ prolapse reconstructive surgery on midurethral sling procedure outcome. Ginekol Pol. 2018;89(4):190–195. https://journals.viamedica.pl/....
22.
Law TSM, Cheung RYK, Chung TKH, et al. Efficacy and outcomes of transobturator tension-free vaginal tape with or without concomitant pelvic floor repair surgery for urinary stress incontinence: five-year follow-up. Hong Kong Med J. 2015;21(4):333–338. https://www.hkmj.org/abstracts....
23.
Anger JT, Litwin MS, Wang Q, et al. The effect of concomitant prolapse repair on sling outcomes. J Urol. 2008;180(3):1003–1006. https://doi.org/10.1016/j.juro....
24.
Rac G, Younger A, Clemens JQ, et al. Stress urinary incontinence surgery trends in academic female pelvic medicine and reconstructive surgery urology practice in the setting of the food and drug administration public health notifications. Neurourol Urodyn. 2017;36(4):1155–1160. https://doi.org/10.1002/nau.23....
25.
Shilpa I, Botros SM. Transvaginal mesh: a historical review and update of the current state of affairs in the United States. Int Urogynecol J. 2017;28(4):527–535. https://doi.org/10.1007/s00192....
26.
Skorupska K, Rechberger T, Bogusiewicz M, et al. Current trends in urogynecological surgeries in Poland. Int Urogyn J. 2020;31(8):1627–1632. https://doi.org/10.1007/s00192....
27.
Wlaźlak E, Viereck V, Kociszewski J, et al. Role of intrinsic sphincter deficiency with and without urethral hypomobility on the outcome of tape insertion. Neurourol Urodyn. 2017;36(7):1910–1916. https://doi.org/10.1002/nau.23....
28.
Laterza RM, Halpern K, Ulrich D, et al. Influence of age, BMI and parity on the success rate of midurethral slings for stress urinary incontinence. PLoS ONE. 2018;13(8): e0201167. https://doi.org/10.1371/journa....
29.
Majkusiak W, Pomian A, Horosz E, et al. Demographic risk factors for mid-urethral sling failure. Do they really matter? PLoS One. 2018;13(11): e0207185. https://doi.org?10.1371/journa....
30.
Brennand EA, Tang S, Williamson T, et al. Twelve-month outcomes following midurethral sling procedures for stress incontinence: impact of obesity. BJOG. 2015;122(12):1705–1712. https://doi.org/10.1111/1471-0....
31.
Kokanali M, Cavkaytar S, Kokanali D, et al. A comperative study for short-term surgical outcomes of midurethral sling procedures in obese and non-obese women with stress urinary incontinence. J Obstet Gynaecol. 2016;36(8):1080–1085. https://doi.org/10.1080/014436....
32.
Barco-Castillo C, Plata M, Zuluaga L, et al. Obesity as a risk factor for poor outcomes after sling surgery in women with stress urinary incotinence: A systematic review and meta-analysis. Neurourol Urodyn. 2020;39(8):2153–2160. https://doi.org/10.1002/nau.24....
33.
Fuselier A, Hanberry J, Margaret Lovin J, et al. Obesity and Stress Urinary Incontinence: Impact on Pathophysiology and Treatment. Curr Urol Rep. 2018;19(1):10. https://doi.org/10.1007/s11934....
34.
Boublil V, Ciofu C, Traxer O, et al. Complications of urethral sling procedures. Curr Opin Obstet Gynecol. 2002;5(5):515–520. https://journals.lww.com/co-ob....
35.
Liang ChCh, Hsieh WCh, Huang L. Comparative study of transobturator sling with and without concomitant prolapse surgery for female urodynamic stress incontinence. J Obstet Gynaecol Res. 2018;44(8):1466–1471. https://doi.org/10.1111/jog.13....
36.
Sokol AI, Jelovsek JE, Walters MD, et al. Incidence and predictors of prolonged urinary retention after TVT with and without concurrent prolapse surgery. Am J Obstet Gynecol. 2005;192(5):1537–1543. https://doi.org/10.1016/j.ajog....
37.
Liu HH, KuoHch. Durability of retropubic suburethral sling procedure and predictors for successful treatment outcome in women with stress urinary incontinence. Urology. 2019;131:83–88. https://doi.org/10.1016/j.urol....
38.
Kuprasertkul A, Zimmen P. Challenges of very long-term reporting in stress urinary incontinence surgeries in women. Urology. 2020;139:50–59. https://doi.org/10.1016/j.urol....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.