Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
National trends in influenza mortality in Poland from 2009–2023 with regard to the periods before, during and after the COVID-19 pandemic
1
Department of Epidemiology, Institute of Rural Health, Lublin, Poland
2
Department of Social Medicine and Public Health, Medical University, Warsaw, Poland
These authors had equal contribution to this work
Corresponding author
Monika Kaczoruk
Institute of Rural Health in Lublin, Institute of Rural Health in Lublin, Jaczewskiego 2, 20-090, Lublin, Poland
Institute of Rural Health in Lublin, Institute of Rural Health in Lublin, Jaczewskiego 2, 20-090, Lublin, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
In the 21st century two pandemics occurred, caused by viral respiratory infections. Both influenza and COVID-19 viruses exhibit high infectivity, have a rapid onset and mutate easily. Considering the fact that the influenza virus is characterized by rotational circulation of strains, while SARS-CoV-2 is constantly evolving, the difficulty is to effectively control the transmission. The extension of lifespan and the emergence of new diseases emphasize the need to assess the risk of death in endemic diseases. The aim of the study is determination of the scale and conditioning of mortality due to influenza in Poland in pre-Covid, Covid, and post-Covid years.
Material and methods:
The study is a retrospective analysis of public statistics data concerning the causes of deaths. The data analyzed were obtained from the Central Statistical Office.
Results:
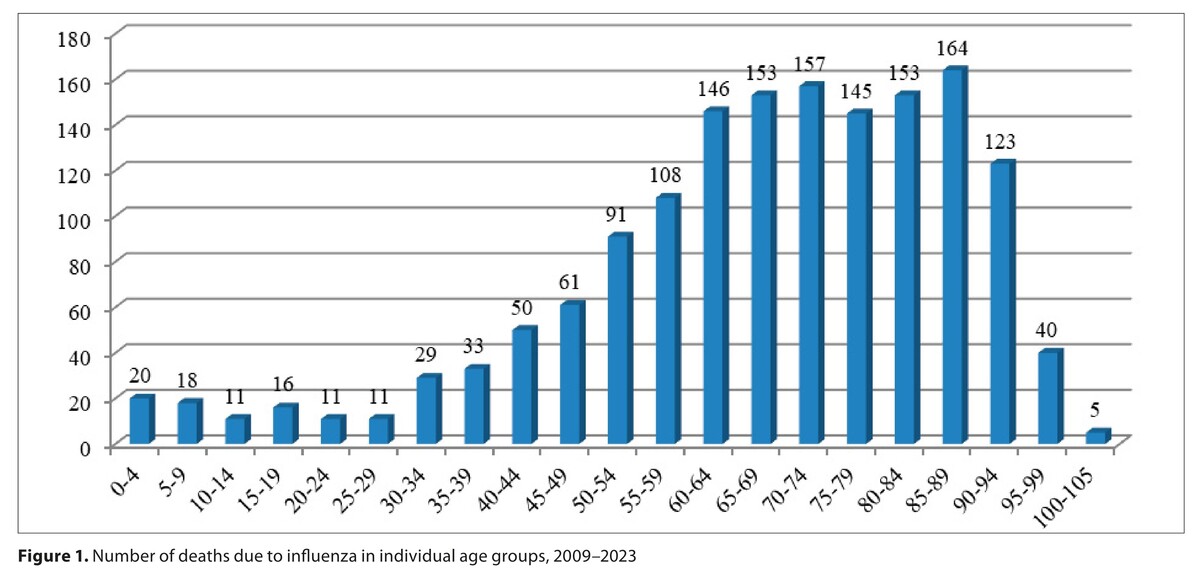
In Poland during 2009 – 2023, 1,545 deaths due to influenza were registered, of which 875 in the pre-Covid period, and 670 during the Covid and post-Covid periods. During the COVID-19 pandemic the incidence of influenza significantly decreased. In Europe, in the season 2022–2023, a four-fold increase in the number of cases of influenza was recorded. In the assessed period of 15 years, the number of deaths among males slightly predominated over that among females, and more than doubled among the urban population, compared to the rural population.
Conclusions:
An increase in life expectancy and the growing threat of emerging diseases has important implications for public health. The national health policy strategy should prioritize and improve vaccination coverage, especially among groups at high risk.
In the 21st century two pandemics occurred, caused by viral respiratory infections. Both influenza and COVID-19 viruses exhibit high infectivity, have a rapid onset and mutate easily. Considering the fact that the influenza virus is characterized by rotational circulation of strains, while SARS-CoV-2 is constantly evolving, the difficulty is to effectively control the transmission. The extension of lifespan and the emergence of new diseases emphasize the need to assess the risk of death in endemic diseases. The aim of the study is determination of the scale and conditioning of mortality due to influenza in Poland in pre-Covid, Covid, and post-Covid years.
Material and methods:
The study is a retrospective analysis of public statistics data concerning the causes of deaths. The data analyzed were obtained from the Central Statistical Office.
Results:
In Poland during 2009 – 2023, 1,545 deaths due to influenza were registered, of which 875 in the pre-Covid period, and 670 during the Covid and post-Covid periods. During the COVID-19 pandemic the incidence of influenza significantly decreased. In Europe, in the season 2022–2023, a four-fold increase in the number of cases of influenza was recorded. In the assessed period of 15 years, the number of deaths among males slightly predominated over that among females, and more than doubled among the urban population, compared to the rural population.
Conclusions:
An increase in life expectancy and the growing threat of emerging diseases has important implications for public health. The national health policy strategy should prioritize and improve vaccination coverage, especially among groups at high risk.
REFERENCES (41)
1.
Li Y, Liu P, Hao T, et al. Rational design of an influenza-COVID-19 chimeric protective vaccine with HA-stalk and S-RBD. Emerg Microbes Infect. 2023;12(2):2231573. doi:10.1080/22221751.
2.
Daemi HB, Kulyar MF, He X, et al. Progression and Trends in Virus from Influenza A to COVID-19: An Overview of Recent Studies. Viruses. 2021;13(6):1145. Published 2021 Jun 15. doi:10.3390/v13061145.
3.
Toribio-Avedillo D, Gómez-Gómez C, Sala-Comorera L, et al. Monitor ing influenza and respiratory syncytial virus in wastewater. Beyond COVID-19. Sci Total Environ. 2023;892:164495. doi:10.1016/j.scitotenv.2023.164495.
4.
Liang J, Wang Y, Lin Z, He W, et al. Influenza and COVID-19 co-infection and vaccine effectiveness against severe cases: a mathematical modeling study. Front Cell Infect Microbiol. 2024;4(14):1347710. doi:10.3389/fcimb.2024.1347710.
5.
Baral SD, Rucinski KB, Twahirwa Rwema JO, et al. The Relationship Between the Global Burden of Influenza From 2017 to 2019 and COVID-19: Descriptive Epidemiological Assessment. JMIR Public Health Surveill. 2021;7(3):e24696. doi:10.2196/24696.
6.
Karimizadeh Z, Dowran R, Mokhtari-azad T, et al. The reproduction rate of severe acute respiratory syndrome coronavirus 2 different variants recently circulated in human: a narrative review. Eur J Med Res. 2023;28(94). doi:https://doi.org/10.1186/s40001....
7.
European Centre for Disease Prevention and Control (ECDC), Factsheet About Seasonal Influenza https://www.ecdc.europa.eu/en/... (access: 2025.08.06).
8.
Pitter JG, Mihajlović J, Nagy D, et al. Underreported influenza mortality in Central and Eastern Europe hinders the extension of seasonal influenza vaccination programs in older adults. Vaccine. 2025;22(56):127184. doi:10.1016/j.vaccine.2025.127184.
9.
Jain R, Sharma H, Pena L, et al. Influenza virus: Genomic insights, evolution, and its clinical presentation. Microb Pathog. 2025;205:107671. doi:10.1016/j.micpath.2025.107671.
10.
World Health Organization. Coronavirus disease (COVID-19) pandemic https://www.who.int/europe/eme... (access: 2025.08.06).
11.
Kang M, Wang LF, Sun BW, et al. Zoonotic infections by avian influenza virus: changing global epidemiology, investigation, and control. Lancet Infect Dis. 2024;24:e522–e531. doi:10.1016/S1473-3099(24)00234-2.
12.
WHO declares that H1N1 pandemic is officially over. BMJ. 2010;341:c4393. doi:https://doi.org/10.1136/bmj.c4....
13.
Han Y, Wang Z, Li X, Zhong Z. Differences of the Chest Images Between Coronavirus Disease 2019 (COVID-19) Patients and Influenza Patients: A Systematic Review and Meta-analysis. Int J Med Sci. 2025;22(3):641–650. doi:10.7150/ijms.98194.
14.
Staadegaard L, Taylor RJ, Spreeuwenberg P, et al. Monitoring the mortality impact of COVID-19 in Europe: What can be learned from 2009 influenza H1N1p mortality studies? Int J Infect Dis. 2020;16;S1201–9712(20)32241–4. doi:10.1016/j.ijid.2020.10.037.
15.
Kanecki, K, Lewtak K, Tyszko P, et al. Hospitalizations and In-Hospital Fatality Among Influenza Patients in the Pre-Pandemic and COVID-19 Pandemic Periods. J Clin Med. 2025;14:1785. https://doi.org/10.3390/jcm140....
16.
Martínez-Baz I, Navascués A, Trobajo-Sanmartín C, et al. Effectiveness of influenza vaccination in preventing confirmed influenza cases and hospitalizations in Northern Spain, 2023/24 season: A population-based test-negative case-control study. Int J Infect Dis. 2025;151:107364. https://doi.org/10.1016/j.ijid....
17.
Nitsch-Osuch A, Jankowski P, Kokoszka-Paszkot J, et al. Towards better protection of older people against influenza and its complications. Polish recommendations for HD influenza vaccine. Fam Med Primary Care Rev. 2024;26(1):116–122. doi:10.5114/fmpcr.2024.134715.
18.
World Health Organization. COVID-19 epidemiological update – 16 February 2024. https://www.who.int/publicatio... (access: 2025.08.06).
19.
Akin L, Gözel MG. Understanding dynamics of pandemics. Turk J Med Sci. 2020;50(SI-1):515–519. https://doi:10.3906/sag-2004-1....
20.
Petti S, Cowling BJ. Ecologic association between influenza and COVID-19 mortality rates in European countries. Epidemiol Infect. 2020;148:e209. https://doi:10.1017/S095026882....
21.
Echevarría-Zuno S, Mejía-Aranguré JM, Mar-Obeso AJ, et al. Infection and death from influenza A H1N1 virus in Mexico: a retrospective analysis. The Lancet. 2009;374(9707), 2072–2079. https://doi.org/10.1016/s0140-....
22.
European Centre for Disease Prevention and Control. Influenza in Europe 2011–2012 surveillance report. https://www.ecdc.europa.eu/en/... (access: 2025.08.06).
23.
European Centre for Disease Prevention and Control. The 2009 A(H1N1) pandemic in Europe Stockholm: ECDC; 2010. https://www.ecdc.europa.eu/sit... (access: 2025.08.06).
24.
Eurostat. Population density by NUTS 3 region. https://ec.europa.eu/eurostat/... (access: 2025.08.06).
25.
World Health Organization Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020 https://www.who.int/dg/speeche... (access: 2025.08.06).
26.
Kondratiuk K, Poznańska A, Szymański K, Czajkowska E, et al. Occurrence of Circulating Antibodies against the Hemagglutinins of Influenza Viruses in the 2022/2023 Epidemic Season in Poland. Viruses. 2024;16(7):1105. https://doi:10.3390/v16071105.
27.
Zachorowania na wybrane choroby zakaźne w Polsce od 1 stycznia do 31 stycznia 2025 r. oraz w porównywalnym okresie 2024 r. Zakład Epidemiologii Chorób Zakaźnych i Nadzoru NIZP PZH – PIB. Departament Zapobiegania i Kontroli Chorób Zakaźnych GIS.
28.
Rzymski P. Projekt FluTer. Wstępna analiza hospitalizacji z powodu grypy w sezonie 2024/2025. 8. Forum Wirusologiczne 2025 March 14–15; Warszawa; 2025.
29.
Rzymski P, Piekarska A, Pleśniak R, et al. Unraveling Poland’s unprecedented influenza surge in early 2025: increased viral severity or post-pandemic vulnerability? Pharmacol Rep. 2025;77(4):1134–1141. https://doi:10.1007/s43440-025....
30.
Rzymski P, Pleśniak R, Piekarska A, et al. Tracking clinical severity of influenza in adult hospitalized patients in 2024: Data from the FluTer registry in Poland. Vaccine. 2025;61,127443. https://doi.org/10.1016/j.vacc....
31.
Sobierajski T, Rzymski P, Wanke-Rytt M. The Influence of Recommendation of Medical and Non-Medical Authorities on the Decision to Vaccinate against Influenza from a Social Vaccinology Perspective: Cross-Sectional, Representative Study of Polish Society. Vaccines (Basel). 2023;11(5):994. https://doi:10.3390/vaccines11....
33.
Meijs DAM, van Bussel BCT, Stessel B, et al. Better COVID-19 Intensive Care Unit survival in females, independent of age, disease severity, comorbidities, and treatment. Scientific Reports. 2022;12 (1):734. https://doi:10.1038/s41598-021....
34.
Heise L, Greene ME, Opper N, et al. Gender Equality, Norms, and Health Steering Committee. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. 2019;15,393(10189):2440–2454. https://doi:10.1016/S0140-6736....
35.
Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R. Klein Impact of sex and gender on COVID-19 outcomes in Europe Biology of Sex Differences. 2020;11(1):29, doi:10.1186/s13293-020-00304-9.
36.
Auderset D, Riou J, Clair C, et al. Why gender and sex matter in infectious disease modelling: A conceptual framework. SSM Popul Health. 2025;12(30):101775. doi:10.1016/j.ssmph.2025.101775.
37.
Naudé W, Nagler P. COVID-19 and the city: Did urbanized countries suffer more fatalities? Cities. 2022;131:103909. doi:10.1016/j.cities.2022.103909.
38.
Tsiotas D, Tselios V. Understanding the uneven spread of COVID-19 in the context of the global interconnected economy. Science Reports. 2022;12(666). doi:10.1038/s41598-021-04717-3.
39.
Han S, Su B, Zhao Y, et al. Widening rural-urban gap in life expectancy in China since COVID-19. BMJ Glob Health. 2023;8(9):e012646. doi:10.1136/bmjgh-2023-012646.
40.
Pruszyński J, Cianciara D, Grudziąż-Sękowska J, et al. Czy w nieodległej przyszłości można spodziewać się ponownej dominacji chorób zakaźnych? J Educ Health Sport. 2022;12(9):658–676. doi:10.12775/JEHS.2022.12.09.079.
41.
Hernandez-Ruiz V, Letenneur L, Fülöp T, et al. Infectious diseases and cognition: do we have to worry? Neurol Sci. 2022;43(11):6215–6224. doi:10.1007/s10072-022-06280-9.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.