Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Hand hygiene as the basic method of reducing Clostridium difficile infections (CDI) in a hospital
environment
1
Project InterDoktorMen, Medical University of Lodz, Poland
2
Laboratory of Epidemiology, Military Institute of Hygiene and Epidemiology (WIHE), Warsaw, Poland
3
University of Technology, Institute of Environmental Engineering, Poznan, Poland
4
Department of Management and Logistics in Health Care, Medical University of Lodz, Poland
Corresponding author
Ann Agric Environ Med. 2021;28(4):535-540
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Clostridium difficile spores, due to their ability to adapt to adverse conditions in a hospital environment, cause enormous difficulties associated with the effective decontamination of surfaces and equipment. Elimination of this pathogen is possible through effective implementation of the hand hygiene procedure by all hospital employees. Scientific research indicates that a properly adopted hand washing procedure reduces the risk of Clostridium difficile infection (CDI) by half.
Objective:
The aim of the study was to indicate the sources of nosocomial infections, mainly Clostridium difficile infection, and methods to limit them, with particular attention paid to the proper hand hygiene of the medical staff, which plays a fundamental role in the transmission of infections between hospitalized patients.
Brief description of the state of knowledge:
Epidemiological studies indicate that about a half of Healthcare Associated Infection (HAI) is caused by microbes that contaminate the hands of medical personnel. One of the main pathogens is Clostridium difficile, which in 2018 in Poland accounted for 41.52% of all detected outbreaks originating from the hospital environment. According to data from WHO,16 million people worldwide die from Healthcare Associated Infection every year, of which approximately 17% constitutes mortality among people infected with Clostridium difficile.
Conclusions:
Non-compliance with hand hygiene among members of medical staff contributes to nosocomial infections which are a major cause of disease complications and deaths. Proper hand hygiene is a key measure for reducing this phenomenon. In every medical institution, especially in hospitals, and staff should be reminded about it and trained to perform the correct hand hygiene technique.
Clostridium difficile spores, due to their ability to adapt to adverse conditions in a hospital environment, cause enormous difficulties associated with the effective decontamination of surfaces and equipment. Elimination of this pathogen is possible through effective implementation of the hand hygiene procedure by all hospital employees. Scientific research indicates that a properly adopted hand washing procedure reduces the risk of Clostridium difficile infection (CDI) by half.
Objective:
The aim of the study was to indicate the sources of nosocomial infections, mainly Clostridium difficile infection, and methods to limit them, with particular attention paid to the proper hand hygiene of the medical staff, which plays a fundamental role in the transmission of infections between hospitalized patients.
Brief description of the state of knowledge:
Epidemiological studies indicate that about a half of Healthcare Associated Infection (HAI) is caused by microbes that contaminate the hands of medical personnel. One of the main pathogens is Clostridium difficile, which in 2018 in Poland accounted for 41.52% of all detected outbreaks originating from the hospital environment. According to data from WHO,16 million people worldwide die from Healthcare Associated Infection every year, of which approximately 17% constitutes mortality among people infected with Clostridium difficile.
Conclusions:
Non-compliance with hand hygiene among members of medical staff contributes to nosocomial infections which are a major cause of disease complications and deaths. Proper hand hygiene is a key measure for reducing this phenomenon. In every medical institution, especially in hospitals, and staff should be reminded about it and trained to perform the correct hand hygiene technique.
REFERENCES (48)
1.
Tolera M, Abate D, Dheresa M, Marami D. Bacterial Nosocomial Infections and Antimicrobial Susceptibility Pattern among Patients Admitted at Hiwot Fana Specialized University Hospital, Eastern Ethiopia. Advances in Medicine. 2018; 1–7. https://doi: 10.1155/2018/2127814.
2.
Cichońska M. Professional solutions in the hygiene of the hands of the medical staff, increasing the effectiveness of fighting hospital infections. Zakażenia XXI wieku. 2019; 2(5): 249–252. https://doi: 10.31350/zakazenia/2019/5/Z2019039.
3.
Łoś I, Dziewulska J. Knowledge of nursing staff concerning Clostridium difficile. Aspekty zdrowia i choroby. 2018; 3(1): 109–132.
4.
Miętkiewicz S, Nowaczyk B, Dyk D. The role of hand hygiene in the prevention of surgical site infections. Hygeia Public Health. 2018; 53(3): 247–252.
5.
Badurek S, Muszytowski M, Stróżecki P, Manitius J. Clostridium difficile-associated disease in patients with chronic kidney disease. Forum Nefrol. 2016; 9(3): 141–148.
6.
Kiersnowska Z, Lemiech-Mirowska E, Ginter-Kramarczyk D, Kruszelnicka I, Michałkiewicz M, Marczak M. Problems of Clostridium difficile infection (CDI) in Polish healthcare units. AAEM. 2020. https://doi: 10.26444/aaem/119321.
7.
Denisiewicz B. The role of disinfection and handwashing of medical personnel – hands as a reservoir of microorganisms – the role of medical dispensers in maintaining hand hygiene. Zakażenia XXI wieku. 2018; 1(3): 125–128.
8.
Kabała M, Aptekorz M, Martirosian G. The role of hospital environment and the hands of medical staff in the transmission of the Clostridioides (Clostridium) difficile infection. Med Pr. 2019; 70(6): 739–745. https://doi: 10.13075/mp.5893.00856.
9.
Dorodgar S, Hatami H, Yadegarynia D, Arab-Mazar Z. Nosocomial Infections: Multicenter Surveillance of Antimicrobial Resistance in Tehran During 2015–2017. Arch Clin Infect Dis. 2018; 13(5): e64246. https://doi: 10.5812/archcid.64246.
10.
Czarkowski MP, Cieleba E, Kondej B, Sadłocha A. Infectious diseases and poisonings in Poland in 2018. Warsaw: National Institute of Public Health – National Institute of HygieneDepartment of Epidemiology and Surveillance of Infectious Diseases; 2019. p. 17–19.
11.
Pawlik K. Clostridiodes (clostridium) difficile – effective infection control methods. Forum Zakażeń. 2018; 9(4): 221–227. https://doi: 10.15374/FZ2018043.
12.
Nowacka K, Flitta R, Siminska J, Porzych P, Grzyb S, Hagner W. Hand hygiene for the management of a patient infected with Clostridium difficile in the presence of hospital infections. Journal of Education, Health and Sport. 2017; 7(6): 331–344. http://doi: 10.5281/zenodo.815567.
13.
The sanitary condition of the country in 2018. Główny Inspektorat Sanitarny. 2019. www.gis.gov.pl (10.04.2020).
14.
McFarland LV, Mulligan ME, Kwok RY, Stamm WE. Nosocomial acquisition of Clostridium difficile infection. N Engl J Med. 1989; 320(4): 204–210. https://doi: 10.1056/NEJM198901263200402.
15.
World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: a Summary. 2009. WHO Press, World Health Organization, Geneva, Switzerland. https://www.cmj.org.pl/clean-c... (5.05.2020).
16.
Goślińska-Kuźniarek O, Karpiński TM. Role of hand hygiene among heathcare personnel. Forum Zakażeń. 2014; 5(2): 79–84.
17.
Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev. 2004; 17(4): 863–893. https://doi: 10.1128/CMR.17.4.863-893.2004.
18.
WHO Guidelines on Hand Hygiene in Health Care. First Global Patient Safety Challenge Clean Care is Safer Care. 2009. WHO Press, World Health Organization, Geneva, Switzerland. ISBN 978 92 4 159790 6.
19.
Piwowarczyk J. Hand hygiene control – Hygiene control in medical facilities. MediNews Information for Professionals of Epidemiology. 2019; 4(1/2019): 7–9. https://www.medilab.pl/userfil... (1.10.2020).
20.
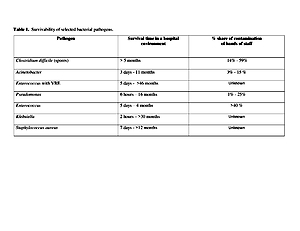
Otter JA, Yezli S, Salkeld JAG, French GL. Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control. 2013; 41: 6–11.
21.
Knape L, Hambraeus A, Lytsy B. The adenosine triphosphate method as a quality control tool to assess ‘cleanliness’ of frequently touched hospital surfaces. J Hosp Infect. 2015; 91(2): 166–170. https://doi:10.1016/j.jhin.20 15.06.011.
22.
Barbut F. How to eradicate Clostridium difficile from the environment. J Hosp Infect. 2015; 89(4): 287–295. https:// doi.org/10.1016/j.jhin.2014.12.007.
23.
Cichońska M, Ciemienga E, Daciąg D, Borek M. The level of knowledge and awareness of medical staff on the subject of hand hygiene. Forum Zakażeń. 2019; 10(4): 227–231. https://doi: 10.15374/FZ2019034.
24.
Tartari E, Muthukumaran P, Peters A, Allegranzi B, Pittet D. Monitoring your institution: the WHO hand hygiene self-assessment frameworkdis it worth it? Clin Microbiol Infect. 2019; 25: 925–928.
25.
Mamos AR, Lipińska D, Orszulak-Michalak DE. Analysis of registered nosocomial infections at the district hospital in the Łódź region 2005–2015. Polish Review of Health Sciences. 2018; 3(56): 294–300.
26.
Niecwietajewa I, Pracz W, Giemza M, Jakubiak J, Szymańczak M, Marusza W. Hand hygiene microbiological control as an important part of multimodal approach for hai prevention. Zakażenia XXI wieku. 2018; 1(5): 209–215. https://doi: 10.31350/zakazenia/2018/5/Z2018036.
27.
Shi L-s, Xu C-j, Jia H-b, Chen W, Zhou X-f, Li X-h. Spread of Staphylococcus aureus between medical staff and high-frequency contact surfaces in a large metropolitan hospital. Int J Nurs Sci. 2015; 2(4): 366–370. https://doi: 10.1016/j.ijnss.2015.11.001.
28.
Bhatt J, Collier S. Reducing Health Care–Associated Infection: Getting Hospitals and Health Systems to Zero. Ann Intern Med. 2019; 171: 81–82. https://doi: 10.7326/M18–3441.
29.
Szumska E. How to properly prepare the hands of the procedure, that the policy of “anything below the elbow”. MediNews. 2018; 3: 12–13. https://www.medilab.pl/userfil.... (1.10.2020).
30.
Khan HA, Baig FK, Mehboob R. Nosocomial infections: Epidemiology, prevention, control and surveillance. Asian Pac J Trop Biomed. 2017; 7(5): 478–482. https://doi: 10.1016/j.apjtb.2017.01.019.
31.
Haque M, Sartelli M, McKimm J, Bakar MA. Health care-associated infections – an overview. Infect Drug Resist. 2018; 11: 2321–2333. https://doi: 10.2147/IDR.S177247.
32.
European standard EN 1499. Chemical disinfectants and antiseptics. Hygienic hand wash. Test method and requirements. Brussels, European Committee for Standardization, 1997.
33.
European standard EN 1500. Chemical disinfectants and antiseptics. Hygienic handrub. Test method and requirements. Brussels, European Committee for Standardization, 1997.
34.
ASTM International. Standard test method for determining the bacteria-eliminating effectiveness of hygienic handwash and handrub agents using the finger pads of adult subjects. 2003 (designation: E 2276).
35.
ASTM International. Standard test method for determining fungus-eliminating effectiveness of hygienic handwash and handrub agents using fingerpads of adults. 2008 (designation: E 2613).
36.
ASTM International. Standard test method for evaluation of handwashing formulations for virus-eliminating activity using the entire hand. 1999 (designation: E 2011).
37.
Potocka P, Rożkiewicz D, Ołdak E. Hand hygiene among healthcare personnel – what else we can do. Forum Zakażeń. 2016; 7(4): 289–293. https://doi: 10.15374/FZ2016050.
38.
Seto WH, Yuen SW, Cheung CW, Ching PT, Cowling BJ, Pittet D. Hand hygiene promotion and the participation of infection control link nurses: an effective innovation to overcome campaign fatigue. Am J Infect Control. 2013; 41(12): 1281–1283. https://doi: 10.1016/j.ajic.2013.04.011.
39.
Kosonóg K, Gotlib J. Assessment of nurses’ familiarity with the principles of aseptics and antiseptics in selected medical procedures. Nursing Problems. 2010; 18(1): 30–40.
40.
Kaier K, Mutters NT, Frank U. Bed occupancy rates and hospital-acquired infections – should beds be kept empty? Clin Microbiol Inf. 2012; 18(10): 941–945. https:// doi: 10.1111/j.1469-0691.2012.03956.x.
41.
Lambe KA, Lydon S, Caoimhe M, Akke V, Aoife H, Walsh M, O’Connor P. Hand Hygiene Compliance in the ICU: A Systematic Review. Critical Care Medicine. 2019; 47(9): 1251–1257. https://doi: 10.1097/CCM.0000000000003868.
42.
Turaga KK, Bhagavatula G. What should doctors wear? BMJ 2008; 337:a938. https://doi.org/10.1136/bmj.a9....
43.
Škodová M, Urra FG, Benítez AG, Romano MRJ, Oritz AG. Hand hygiene assessment in the workplace using a UV lamp. Am J Infect Control. 2015; 43(12): 1360–1362. https://doi: 10.1016/j.ajic.2015.07.003.
44.
McNeil SA, Foster CL, Hedderwick SA, Kauffman CA. Effect of hand cleansing with antimicrobial soap or alcohol-based gel on microbial colonization of artificial fingernails worn by health care workers. Clin Infect Dis. 2001; 32(3): 367–372. https://doi: 10.1086/318488.
45.
Moolenaar RL, Crutcher JM, San Joaquin VH, Sewell LV, Hutwagner LC, Carson LA, Robison DA, Smithee LM, Jarvis WR. A prolonged outbreak of Pseudomonas aeruginosa in a neonatal intensive care unit: did staff fingernails play a role in disease transmission? Infect Control Hosp Epidemiol. 2000; 21(2): 80–85. https://doi: 10.1086/501739.
46.
Gupta A, Della-Latta P, Todd B, Gabriel PS, Haas J, Wu F, Rubenstein D, Saiman L. Outbreak of extended spectrum beta-lactamase-producing Klebsiella pneumoniae in a neonatal intensive care unit linked to artificial nails. Infect Control Hosp Epidemiol. 2004; 25(3): 210–215. https://doi: 10.1086/502380.
47.
Weber RL, Khan PD, Fader RC, Weber RA. Prospective study on the effect of shirt sleeves and ties on the transmission of bacteria to patients. J Hosp Infect. 2012; 80(3): 252–254. https://doi: 10.1016/j.jhin.2011.12.012.
48.
Khan R, Petersen FC, Shekhar S. Commensal Bacteria: An Emerging Player in Defense Against Respiratory Pathogens. Front Immunol. 2019; 10, 1203. https://doi.org/10.3389/fimmu.....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.