Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Dyslipidaemia, carbohydrate metabolism disorders and arterial hypertension detected in academic employees during examinations in occupational medicine
1
Department of Occupational Diseases and Environmental Health, Nofer Institute of Occupational Medicine, Łódź, Poland
2
III Department of Internal Diseases and Cardiology, Medical University of Warsaw, Poland
3
Department of Public Health, Medical University of Warsaw, Poland
4
Department of Internal Medicine and Cardiology, Municipal Hospital in Olsztyn, Poland
5
Department of Environmental Epidemiology, Nofer Institute of Occupational Medicine, Łódź, Poland
6
Department of Experimental and Clinical Pharmacology, Medical University of Warsaw, Poland
7
1st Department of Cardiology, Interventional Electrocardiology and Hypertension, Institute of Cardiology, Jagiellonian University Medical College, Kraków, Poland
Corresponding author
Andrzej Marcinkiewicz
Nofer Institute of Occupational Medicine, Św. Teresy od Dzieciątka Jezus 8, 91-348, Łódź, Poland
Nofer Institute of Occupational Medicine, Św. Teresy od Dzieciątka Jezus 8, 91-348, Łódź, Poland
Ann Agric Environ Med. 2021;28(2):314-318
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Many people have CVD risk factors without realising it and it is important to recognise the risk factors as soon as possible. Periodic examinations are a mandatory form of control for all employes in Poland. They provide an excellent opportunity to screen for the most common civilization diseases in the population.
Objective:
The aim of this study is to evaluate the prevalence of dyslipidaemia, hyperglycaemia and hypertension among academics in a Polish university, and to compare the results between postdoctoral fellows and other academics.
Material and methods:
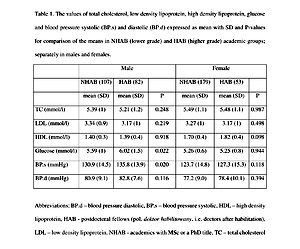
The study group were postdoctoral fellows (HAB; N=135, 53 females) and other academics (NHAB; N=286, 179 females) over the age of 40 who reported for a periodic occupational medical check-up. Fasting blood samples were drawn, serum glucose, lipids and blood pressure (BP) were measured.
Results:
The mean age was 56.7 (SD 9.8) in HAB and 49.8 (SD 8.1) in NHAB. Mean systolic BP and glycaemia were significantly higher in male HAB group than male NHAB (135.8 vs 130.9 mmHg and 6.0 vs 5.6 mmol/l, respectively). The relationship in females was non-significant. The age-adjusted odds ratios (OR [95% CI]) of having elevated low density lipoprotein cholesterol, total cholesterol, glucose and blood pressure in male HAB vs male NHAB were 0.61 [0.32. 1.16], 0.64 [0.33, 1.23], 1.52 [0.80, 2.88] and 2.11 [0.88, 5.23], and in female HAB vs female NHAB – 0.59 [0.31, 1.12], 0.64 [0.32, 1.26], 0.87 [0.40, 1.79] and 1.86 [0.70, 4.68], respectively.
Conclusions:
Adequately planned occupational medicine examinations provide an opportunity to diagnose dyslipidaemia, hyperglycaemia, or high BP in all groups of employees, including highly educated academics.
Many people have CVD risk factors without realising it and it is important to recognise the risk factors as soon as possible. Periodic examinations are a mandatory form of control for all employes in Poland. They provide an excellent opportunity to screen for the most common civilization diseases in the population.
Objective:
The aim of this study is to evaluate the prevalence of dyslipidaemia, hyperglycaemia and hypertension among academics in a Polish university, and to compare the results between postdoctoral fellows and other academics.
Material and methods:
The study group were postdoctoral fellows (HAB; N=135, 53 females) and other academics (NHAB; N=286, 179 females) over the age of 40 who reported for a periodic occupational medical check-up. Fasting blood samples were drawn, serum glucose, lipids and blood pressure (BP) were measured.
Results:
The mean age was 56.7 (SD 9.8) in HAB and 49.8 (SD 8.1) in NHAB. Mean systolic BP and glycaemia were significantly higher in male HAB group than male NHAB (135.8 vs 130.9 mmHg and 6.0 vs 5.6 mmol/l, respectively). The relationship in females was non-significant. The age-adjusted odds ratios (OR [95% CI]) of having elevated low density lipoprotein cholesterol, total cholesterol, glucose and blood pressure in male HAB vs male NHAB were 0.61 [0.32. 1.16], 0.64 [0.33, 1.23], 1.52 [0.80, 2.88] and 2.11 [0.88, 5.23], and in female HAB vs female NHAB – 0.59 [0.31, 1.12], 0.64 [0.32, 1.26], 0.87 [0.40, 1.79] and 1.86 [0.70, 4.68], respectively.
Conclusions:
Adequately planned occupational medicine examinations provide an opportunity to diagnose dyslipidaemia, hyperglycaemia, or high BP in all groups of employees, including highly educated academics.
REFERENCES (29)
1.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J [Internet]. 2019; 41: 111–88. Available from: https://doi.org/10.1093/eurhea....
2.
Wijeysundera HC, Machado M, Farahati F, Wang X, Witteman W, van der Velde G, et al. Association of temporal trends in risk factors and treatment uptake with coronary heart disease mortality, 1994–2005. JAMA. United States; 2010; 303: 1841–7.
3.
Goff DC Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, et al. Dyslipidemia Prevalence, Treatment, and Control in the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation [Internet]. American Heart Association; 2006; 113: 647–56. Available from: https://doi.org/10.1161/CIRCUL....
4.
Yu OHY, Suissa S. Identifying Causes for Excess Mortality in Patients With Diabetes: Closer but Not There Yet. Diabetes Care [Internet]. 2016; 39: 1851 LP – 1853. Available from: http://care.diabetesjournals.o....
5.
Zdrojewski T, Solnica B, Cybulska B, Bandosz P, Rutkowski M, Stokwiszewski J, et al. Prevalence of lipid abnormalities in Poland. The NATPOL 2011 survey. Kardiol Pol. Poland; 2016; 74: 213–23.
6.
Topor-Madry R, Wojtyniak B, Strojek K, Rutkowski D, Bogusławski S, Ignaszewska-Wyrzykowska A, et al. Prevalence of diabetes in Poland: a combined analysis of national databases. Diabet Med. England; 2019; 36: 1209–16.
7.
Rutkowski M, Bandosz P, Czupryniak L, Gaciong Z, Solnica B, Jasiel-Wojculewicz H, et al. Prevalence of diabetes and impaired fasting glucose in Poland – the NATPOL 2011 Study. Diabet Med. England; 2014; 31: 1568–71.
8.
Małyszko J, Mastej M, Banach M, Tykarski A, Narkiewicz K, Hoffman P, et al. Do we know more about hypertension in Poland after the May Measurement Month 2017? – Europe. Eur Hear J Suppl [Internet]. 2019; 21: D97–100. Available from: https://doi.org/10.1093/eurhea....
9.
Marcinkiewicz A. Zasoby i działalność jednostek służby medycyny pracy w Polsce. Analiza obligatoryjnej sprawozdawczości za lata 2014–2018. Med Pr. 2020; 71.
10.
Czerwińska K, Gać P, Poręba R, Mazur G, Pawlas K. Cardiac and vascular disorders as para-occupational diseases – a Polish perspective. Ann Agric Environ Med [Internet]. 2020; Available from: http://dx.doi.org/10.26444/aae....
11.
Krzowski B, Płatek AE, Szymański FM, Ryś A, Semczuk-Kaczmarek K, Adamkiewicz K, et al. Epidemiology of dyslipidaemia in professional drivers: results of RACER-ABPM (Risk of Adverse Cardiovascular Events among professional dRivers in Poland – Ambulatory Blood Pressure Monitoring) study. Kardiol Pol. Poland; 2018; 76: 396–400.
12.
Mirmohammadi SJ, Taheri M, Mehrparvar AH, Heydari M, Saadati Kanafi A, Mostaghaci M. Occupational stress and cardiovascular risk factors in high-ranking government officials and office workers. Iran Red Crescent Med J [Internet]. 2014/08/01. Kowsar; 2014; 16: e11747–e11747. Available from: https://pubmed.ncbi.nlm.nih.go....
13.
Ofori SN, Obosi J. Prevalence of hypertension among office workers in a multi-national company in the Niger-Delta with the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines. Prev Med reports [Internet]. Elsevier; 2019; 15: 100899. Available from: https://pubmed.ncbi.nlm.nih.go....
14.
Szymański FM, Barylski M, Cybulska B, Wożakowska-Kapłon B, Krasiński Z, Mamcarz A, et al. Recommendation for the management of dyslipidemia in Poland – Third Declaration of Sopot. Interdisciplinary Expert Position Statement endorsed by the Polish Cardiac Society Working Group on Cardiovascular Pharmacotherapy. Cardiol J. Poland; 2018; 25: 655–65.
15.
Piotrowski W, Waskiewicz A, Cicha-Mikolajczyk A. Global cardiovascular mortality risk in the adult Polish population: prospective assessment of the cohorts studied in multicentre national WOBASZ and WOBASZ Senior studies. Kardiol Pol. Poland; 2016; 74: 262–73.
16.
Tsutsumi A, Kayaba K, Tsutsumi K, Igarashi M. Association between job strain and prevalence of hypertension: a cross sectional analysis in a Japanese working population with a wide range of occupations: theJichi Medical School cohort study. Occup Environ Med [Internet]. 2001; 58: 367 LP – 373. Available from: http://oem.bmj.com/content/58/....
17.
Radi S, Lang T, Lauwers-Cances V, Diene E, Chatellier G, Larabi L, et al. Job constraints and arterial hypertension: different effects in men and women: the IHPAF II case control study. Occup Environ Med [Internet]. 2005; 62: 711 LP–717. Available from: http://oem.bmj.com/content/62/....
18.
Cornelia R, Stefan K, Markus T, Guido H. Age and work-related stress: a review and meta-analysis. Guido Hertel Annet H. de Lange, Jürgen Deller BIJM van der H, editor. J Manag Psychol [Internet]. Emerald Group Publishing Limited; 2013; 28: 781–804. Available from: https://doi.org/10.1108/JMP-07....
19.
Fishta A, Backé E-M. Psychosocial stress at work and cardiovascular diseases: an overview of systematic reviews. Int Arch Occup Environ Health [Internet]. 2015/02/17. Springer Berlin Heidelberg; 2015; 88: 997–1014. Available from: https://pubmed.ncbi.nlm.nih.go....
20.
Eades CE, France EF, Evans JMM. Prevalence of impaired glucose regulation in Europe: a meta-analysis. Eur J Public Health [Internet]. 2016; 26: 699–706. Available from: https://doi.org/10.1093/eurpub....
21.
Kim KS, Kim SJ, Kim S, Choi D-W, Ju YJ, Park E-C. Association of self-reported sedentary time with insulin resistance among Korean adults without diabetes mellitus: a cross-sectional study. BMC Public Health [Internet]. 2018; 18: 1335. Available from: https://doi.org/10.1186/s12889....
22.
Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. Germany; 2012; 55: 2895–905.
23.
Kivimäki M, Virtanen M, Kawachi I, Nyberg ST, Alfredsson L, Batty D, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222 120 individuals. lancet Diabetes Endocrinol [Internet]. 2014/09/25. The Lancet, Diabetes & Endocrinology; 2015; 3: 27–34. Available from: https://pubmed.ncbi.nlm.nih.go....
24.
Weinhold KR, Miller CK, Marrero DG, Nagaraja HN, Focht BC, Gascon GM. A Randomized Controlled Trial Translating the Diabetes Prevention Program to a University Worksite, Ohio, 2012–2014. Prev Chronic Dis [Internet]. Centers for Disease Control and Prevention; 2015; 12: E210–E210. Available from: https://pubmed.ncbi.nlm.nih.go....
25.
Zellweger U, Bopp M, Holzer BM, Djalali S, Kaplan V. Prevalence of chronic medical conditions in Switzerland: exploring estimates validity by comparing complementary data sources. BMC Public Health [Internet]. 2014; 14: 1157. Available from: https://doi.org/10.1186/1471-2....
26.
Cho SMJ, Lee HJ, Shim JS, Song BM, Kim HC. Associations between age and dyslipidemia are differed by education level: The Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort. Lipids Health Dis [Internet]. 2020; 19: 12. Available from: https://doi.org/10.1186/s12944....
27.
Ha KH, Kwon H-S, Kim DJ. Epidemiologic Characteristics of Dyslipidemia in Korea. J Lipid Atheroscler [Internet]. Korean Society of Lipidology and Atherosclerosis; 2015; 4: 93–9. Available from: https://doi.org/10.12997/jla.2....
28.
Chmiel C, Bhend H, Senn O, Zoller M, Rosemann T. The FIRE project: a milestone for research in primary care in Switzerland. Swiss Med Wkly. Switzerland; 2011; 140: w13142.
29.
Krztoń-Królewiecka A, Oleszczyk M, Schäfer WLA, Boerma WG, Windak A. Quality of primary health care in Poland from the perspective of the physicians providing it. BMC Fam Pract [Internet]. BioMed Central; 2016; 17: 151. Available from: https://pubmed.ncbi.nlm.nih.go....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.