Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Association between apparent temperature and hypertension hospital admissions: a case study in rural areas in western China
1
School of Economics and Management, University of Technology, Lanzhou, China
2
Institute of Technology, Huaibei, China
3
School of Public and Administration, Chongqing University, China
Corresponding author
Ann Agric Environ Med. 2023;30(3):490-497
KEYWORDS
TOPICS
- Health effects of chemical pollutants in agricultural areas , including occupational and non-occupational effects of agricultural chemicals (pesticides, fertilizers) and effects of industrial disposal (heavy metals, sulphur, etc.) contaminating the atmosphere, soil and water
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
Although it has previously been shown that temperature is associated with cardiovascular disease, no investigations exploring the association between apparent temperature (AT) and hypertension in farmers in Zhangye and Longnan, Gansu Province, China, have been undertaken. As hypertension is a commonly known risk factor for cardiovascular disease, the relationship between apparent temperature (AT) and hypertension is examined in Zhangye and Longnan to provide advice to local governments on preventive measures.
Material and methods:
Daily data and weather conditions were collected in Zhangye and Longnan from 2014–2015. The Poisson generalized linear model and the distributed lag nonlinear model (DLNM) were combined to investigate the relationship between AT and hypertension in hospital admissions in the study areas.
Results:
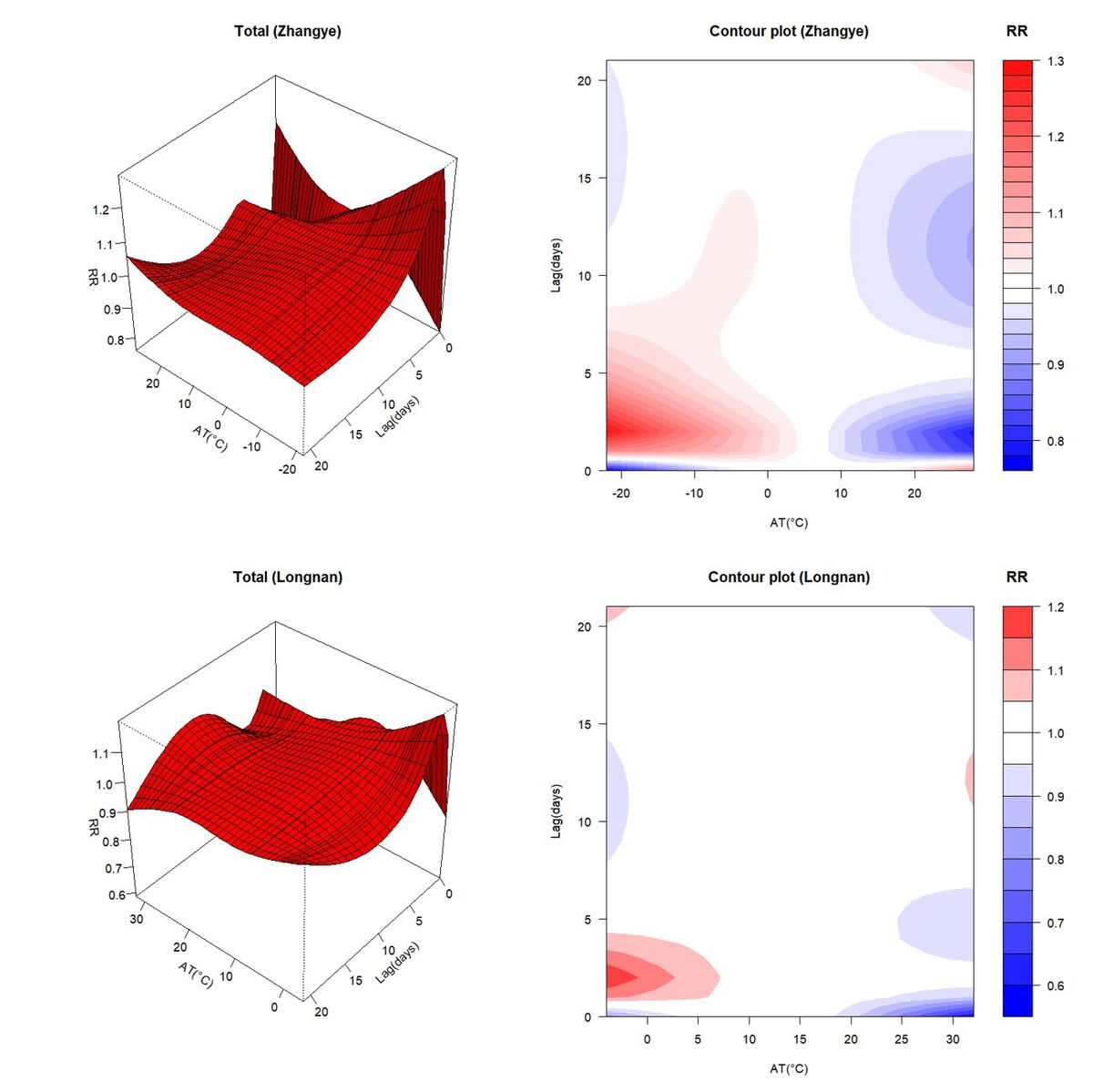
A non-linear relationship between AT and hypertension in hospital admissions in both Zhangye and Longnan were recorded. The cold effects were stronger in Zhangye than that in Longnan for both study group and subgroups. The heat effects were more deleterious for the entire study group, female subgroup and adult subgroup in Longnan, but stronger for the male subgroup and elderly subgroup in Zhangye.
Conclusions:
This investigation indicates that AT has adverse impacts on hypertension hospital admissions in Zhangye and Longnan, especially under low AT exposure levels. The results from this study may promote the formulation of further prevention measures for hypertension disease.
Although it has previously been shown that temperature is associated with cardiovascular disease, no investigations exploring the association between apparent temperature (AT) and hypertension in farmers in Zhangye and Longnan, Gansu Province, China, have been undertaken. As hypertension is a commonly known risk factor for cardiovascular disease, the relationship between apparent temperature (AT) and hypertension is examined in Zhangye and Longnan to provide advice to local governments on preventive measures.
Material and methods:
Daily data and weather conditions were collected in Zhangye and Longnan from 2014–2015. The Poisson generalized linear model and the distributed lag nonlinear model (DLNM) were combined to investigate the relationship between AT and hypertension in hospital admissions in the study areas.
Results:
A non-linear relationship between AT and hypertension in hospital admissions in both Zhangye and Longnan were recorded. The cold effects were stronger in Zhangye than that in Longnan for both study group and subgroups. The heat effects were more deleterious for the entire study group, female subgroup and adult subgroup in Longnan, but stronger for the male subgroup and elderly subgroup in Zhangye.
Conclusions:
This investigation indicates that AT has adverse impacts on hypertension hospital admissions in Zhangye and Longnan, especially under low AT exposure levels. The results from this study may promote the formulation of further prevention measures for hypertension disease.
ABBREVIATIONS
AT – Apparent Temperature; DLNM – Distributed Lag Nonlinear Model; RR – Relative Risk
ACKNOWLEDGEMENTS
The study was supported by the National Natural Science Foundation of China (No. 71861026); the Natural Science Foundation of Gansu Province (No. 20JR10RA149)
and the China Post-doctoral Science Foundation (No. 2016M600827)
REFERENCES (42)
1.
Liu Y, Guo Y, Wang C, et al. Association between temperature change and outpatient visits for respiratory tract infections among children in Guangzhou, China. Int J Environ Res Public Health. 2015; 12(1): 439–454. https://doi.org/10.3390/ijerph....
2.
Ma Y, Zhou J, Yang S, et al. Effects of extreme temperatures on hospital emergency room visits for respiratory diseases in Beijing, China. Environ Sci Pollut Res Int. 2019; 26: 3055–3064. https://doi.org/10.1007/ s11356–018–3855–4.
3.
Mohammadi R, Soori H, Alipour A, et al. The impact of ambient temperature on acute myocardial infarction admissions in Tehran, Iran. J Therm Biol. 2018; 73: 24–31. http://doi.org/10.1016/j. jtherbio.2018.02.008.
4.
Cheng J, Xie M Y, Zhao K F, et al. Impacts of ambient temperature on the burden of bacillary dysentery in urban and rural Hefei, China. Epidemiol Infect. 2017; 145(8): 1567–1576. http://doi.org/10.1017/ S0950268817000280.
5.
Zhao Q, Zhao Y, Li S, et al. Impact of ambient temperature on clinical visits for cardio-respiratory diseases in rural villages in northwest China. Sci Total Environ. 2018; 612: 379–385. http://doi.org/10.1016/j. scitotenv.2017.08.244.
6.
Lavigne E, Gasparrini A, Wang X, et al. Extreme ambient temperatures and cardiorespiratory emergency room visits: assessing risk by comorbid health conditions in a time series study. Environ Health. 2014; 13: 1–8. http://doi.org/10.1186/1476–06....
7.
Tian Z, Li S, Zhang J, et al. Ambient temperature and coronary heart disease mortality in Beijing, China: a time series study. Environ Health. 2012; 11: 1–7. http://doi.org/10.1186/1476–06....
8.
Zhang YH, Chai PP, Zhai TM, et al. Study on accounting and analysis of curative expenditure on cardio-cerebrovascular diseases in China. Chinese Circulation J. 2020.
9.
Yang J, Ou C Q, Ding Y, et al. Daily temperature and mortality: a study of distributed lag non-linear effect and effect modification in Guangzhou. Environ Health. 2012; 11(1): 1–9. http://doi.org/10.1186/1476– 069X-11–63.
10.
Song X, Wang S, Li T, et al. The impact of heat waves and cold spells on respiratory emergency department visits in Beijing, China. Sci Total Environ. 2018; 615: 1499–1505. http://doi.org/10.1016/j. scitotenv.2017.09.108.
11.
Phung D, Guo Y, Thai P, et al. The effects of high temperature on cardiovascular admissions in the most populous tropical city in Vietnam. Environ Pollut. 2016; 208: 33–39. http://doi.org/10.1016/j. envpol.2015.06.004.
12.
Yu W, Hu W, Mengersen K, et al. Time course of temperature effects on cardiovascular mortality in Brisbane, Australia. Heart. 2011; 97(13): 1089–1093. http://doi.org/10.1136/hrt.201....
13.
Chen R, Li T, Cai J, et al. Extreme temperatures and out-of-hospital coronary deaths in six large Chinese cities. J Epidemiol Community Health. 2014; 68(12): 1119–1124. http://doi.org/10.1136/jech-20... 204012.
14.
Sharafkhani R, Khanjani N, Bakhtiari B, et al. Diurnal temperature range and mortality in Tabriz (the northwest of Iran). Urban Climate. 2019; 27: 204–211. http://doi.org/10.1016/j.uclim....
15.
Wang M, Zheng S, He S, et al. The association between diurnal temperature range and emergency room admissions for cardiovascular, respiratory, digestive and genitourinary disease among the elderly: a time series study. Sci Total Environ. 2013; 456: 370–375. http://doi. org/10.1016/j.scitotenv.2013.03.023.
16.
Zheng S, Zhu W, Wang M, et al. The effect of diurnal temperature range on blood pressure among 46,609 people in Northwestern China. Sci Total Environ. 2020; 730: 138987. https://doi.org/10.1016/j. scitotenv.2020.138987.
17.
Niu Y, Gao Y, Yang J, et al. Short-term effect of apparent temperature on daily emergency visits for mental and behavioral disorders in Beijing, China: A time-series study. Sci Total Environ. 2020; 733: 139040. https:// doi.org/10.1016/j.scitotenv.2020.139040.
18.
Yi W, Zhang X, Gao J, et al. Examining the association between apparent temperature and admissions for schizophrenia in Hefei, China, 2005–2014: a time-series analysis. Sci Total Environ. 2019; 672: 1–6. https:// doi.org/10.1016/j.scitotenv.2019.03.436.
19.
Min M, Shi T, Ye P, et al. Effect of apparent temperature on daily emergency admissions for mental and behavioral disorders in Yancheng, China: a time-series study. Environ Health. 2019; 18(1): 1–12. https:// doi.org/10.1186/s12940–019–0543-x.
20.
Moghadamnia M T, Ardalan A, Mesdaghinia A, et al. The effects of apparent temperature on cardiovascular mortality using a distributed lag nonlinear model analysis: 2005 to 2014. Asia Pac J Public Health. 2018; 30(4): 361–368. https://doi.org/10.1177/101053....
21.
Wichmann J, Andersen Z J, Ketzel M, et al. Apparent temperature and cause-specific mortality in Copenhagen, Denmark: A case crossover analysis. Int J Environ Res Public Health. 2011; 8(9): 3712–3727. https://doi.org/10.3390/ijerph....
22.
Moghadamnia M T, Ardalan A, Mesdaghinia A, et al. Association between apparent temperature and acute coronary syndrome admission in Rasht, Iran. Heart Asia. 2018; 10(2). https://doi.org/10.1136/hearta....
23.
Lin X, Du Z, Liu Y, et al. The short-term association of ambient fine particulate air pollution with hypertension clinic visits: A multi-community study in Guangzhou, China. Sci Total Environ. 2021; 774: 145707. https://doi.org/10.1016/j.scit....
24.
Hu J, He G, Luo J, et al. Temperature-adjusted hypertension prevalence and control rate: a series of cross-sectional studies in Guangdong Province, China. J Hypertens. 2021; 39(5): 911–918. https://doi.org/10.1097/HJH.00....
25.
Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018; 137(22): 2344–2356. https://doi.org/10.1161/CIRCUL....
26.
Zhang Y, Liu X, Kong D, et al. Effects of ambient temperature on acute exacerbations of chronic obstructive pulmonary disease: results from a time-series analysis of 143318 hospitalizations. Int J Chron Obstruct Pulmon Dis. 2020; 213–223. http://doi.org/10.2147/COPD.S2....
27.
Meng XY, Zheng S, Wei XF, et al. Effects of cold waves on hospital admissions for hypertension in Jinchang, Gansu Province: A case-crossover study. J Environ Occup Med. 2020; 37(1).
28.
Maria Bruno R, Di Pilla M, Ancona C, et al. Environmental factors and hypertension. Curr Pharmaceutical Design. 2017; 23(22): 3239–3246. https://doi.org/10.2174/138161....
29.
Su D, Du H, Zhang X, et al. Season and outdoor temperature in relation to detection and control of hypertension in a large rural Chinese population. Int J Epidemiol. 2014; 43(6): 1835–1845. https://doi.org/10.1093/ije/dy....
30.
Wang Q, Zhao Q, Wang G, et al. The association between ambient temperature and clinical visits for inflammation-related diseases in rural areas in China. Environ Pollut. 2020; 261: 114128. https://doi.org/10.1016/j.envp....
31.
Phosri A, Sihabut T, Jaikanlaya C. Short-term effects of diurnal temperature range on hospital admission in Bangkok, Thailand. Sci Total Environ. 2020; 717: 137202. https://doi.org/10.1016/j.scit....
32.
Guo S, Niu Y, Cheng Y, et al. Association between ambient temperature and daily emergency hospitalizations for acute coronary syndrome in Yancheng, China. Environ Sci Pollut Res Int. 2020; 27: 3885–3891. https://doi.org/10.1007/s11356....
33.
Wang B, Chai G, Sha Y, et al. Impact of ambient temperature on cardiovascular disease hospital admissions in farmers in China’s Western suburbs. Sci Total Environ. 2021; 761: 143254. https://doi.org/10.1016/j.scit....
34.
Yu B, Jin S, Wang C, et al. The association of outdoor temperature with blood pressure, and its influence on future cardio-cerebrovascular disease risk in cold areas. J Hypertens. 2020; 38(6): 1080–1089. https://doi.org/10.1097/HJH.00....
35.
Lewington S, Lacey B, Clarke R, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016; 176(4): 524–532. https://doi.org/10.1001/jamain....
36.
Zhang X, Zhang S, Wang C, et al. Effects of moderate strength cold air exposure on blood pressure and biochemical indicators among cardiovascular and cerebrovascular patients. Int J Environ Res Public Health. 2014; 11(3): 2472–2487. https://doi.org/10.3390/ijerph....
37.
Fares A. Winter hypertension: potential mechanisms. Inter J Health Sci. 2013; 7(2): 210. https://doi.org/10.12816/00060....
38.
Zheng S, Wang M Z, Cheng Z Y, et al. Effects of outdoor temperature on blood pressure in a prospective cohort of northwest China. Biomed Environ Sci. 2021; 34(2): 89–100. https://doi.org/10.3967/bes202....
39.
Ge Y, Liu C, Niu Y, et al. Associations between ambient temperature and daily hospital admissions for rheumatic heart disease in Shanghai, China. Int J Biometeorol. 2018; 62: 2189–2195. https://doi.org/10.1007/s00484....
40.
Wang X, Li G, Liu L, et al. Effects of extreme temperatures on cause-specific cardiovascular mortality in China. Int J Environ Res Public Health. 2015; 12(12): 16136–16156. https://doi.org/10.3390/ijerph....
41.
Zhai L, Ma X, Wang J, et al. Effects of ambient temperature on cardiovascular disease: A time-series analysis of 229288 deaths during 2009–2017 in Qingdao, China. Int J Environ Health Res. 2022; 32(1): 181–190. https://doi.org/10.1080/096031....
42.
Brook R D. The environment and blood pressure. Cardiology Clin. 2017; 35(2): 213–221. https://doi.org/10.1016/j.ccl.....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.