Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Assessment of the degree of illness acceptance in patients diagnosed with hepatitis C
1
Military Clinical Hospital No. 1 with Polyclinic, Independent Public Health Unit, Lublin, Poland
Corresponding author
Lidia Elżbieta Sierpińska
Military Clinical Hospital No. 1 with Polyclinic, Independent Public Health Unit, Al. Racławicke 23, 20-049, Lublin, Poland
Military Clinical Hospital No. 1 with Polyclinic, Independent Public Health Unit, Al. Racławicke 23, 20-049, Lublin, Poland
Ann Agric Environ Med. 2022;29(2):224-231
KEYWORDS
TOPICS
ABSTRACT
Introduction:
In Poland, approximately 730,000 people are infected with the hepatitis C virus (HCV). Acceptance of a chronic illness may positively motivate patients in the process of treatment. The higher the degree of illness acceptance, the lower the feeling of psychological discomfort and a lower intensity of negative emotions.
Objective:
The aim of the study was assessment of illness acceptance among patients with chronic hepatitis C, and determination of the level of the relationship between social and demographic variables, and the degree of illness acceptance.
Material and methods:
The study included 220 patients with a diagnosis of chronic hepatitis C. The research method was a diagnostic survey, while the instruments used were the Acceptance of Illness Scale (AIS) and an author-constructed questionnaire.
Results:
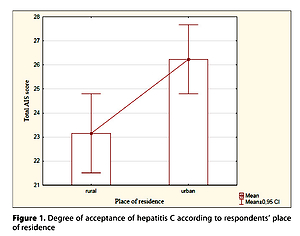
Respondents most frequently accepted their illness to the mean degree (30 scores), and a low category or even the lack of acceptance (<20 scores) of respondents. Urban inhabitants significantly more often accepted their illness to a high degree, compared to rural inhabitants. Disability pensioners and retired pensioners significantly more frequently accepted their disease in the category – low degree. The remaining independent variables: gender, age, education, marital status, number of years of illness, had no significant effect on the degree of acceptance of hepatitis C.
Conclusions:
The majority of patients diagnosed with chronic hepatitis C accept their illness to the mean degree. Patients with hepatitis C should be covered with psychological assistance in order to change the way of perception and evaluation of their health situation in more positive terms.
In Poland, approximately 730,000 people are infected with the hepatitis C virus (HCV). Acceptance of a chronic illness may positively motivate patients in the process of treatment. The higher the degree of illness acceptance, the lower the feeling of psychological discomfort and a lower intensity of negative emotions.
Objective:
The aim of the study was assessment of illness acceptance among patients with chronic hepatitis C, and determination of the level of the relationship between social and demographic variables, and the degree of illness acceptance.
Material and methods:
The study included 220 patients with a diagnosis of chronic hepatitis C. The research method was a diagnostic survey, while the instruments used were the Acceptance of Illness Scale (AIS) and an author-constructed questionnaire.
Results:
Respondents most frequently accepted their illness to the mean degree (30 scores), and a low category or even the lack of acceptance (<20 scores) of respondents. Urban inhabitants significantly more often accepted their illness to a high degree, compared to rural inhabitants. Disability pensioners and retired pensioners significantly more frequently accepted their disease in the category – low degree. The remaining independent variables: gender, age, education, marital status, number of years of illness, had no significant effect on the degree of acceptance of hepatitis C.
Conclusions:
The majority of patients diagnosed with chronic hepatitis C accept their illness to the mean degree. Patients with hepatitis C should be covered with psychological assistance in order to change the way of perception and evaluation of their health situation in more positive terms.
REFERENCES (32)
1.
Zakrzewska K, Szmulik K, Stępień M, et al. Wirusowe zapalenie wątroby typu C w Polsce w 2015 roku. Przegl Epidemiol. 2017; 71(3): 363–371.
2.
Zakrzewska K, Stępień M, Rosińsk M. Wirusowe zapalenie wątroby typu C (wzw C) w Polsce w 2017 roku. Przegl Epidemiol. 2019; 73(2): 167–178. https://doi.org/10.32394/pe.73....
3.
Pokorska-Śpiewak M, Śpiewak M. Management of hepatitis C in children and adolescents during COVID-19 pandemic. World J Hepatol. 2020; 12(8): 485–492. https://doi.org/10.4254/wjh.v1....
4.
Kamili S, Drobeniuc J, Araujo AC, et al. Laboratory diagnostics for hepatitis C virus infection. Clin Infect Dis. 2012; 55(1): 43–48, https://doi.org/10.1093/cid/ci....
5.
Sierpińska L. Hepatitis C as a health problem in Poland. J Nurs Care. 2015; 1(1): 1–5.
6.
Hashim AE, Zaky S, Azab N, et al. Peripheral blood mononuclear cells hepatitis C virus RNA as a predictor for the response to daclatasvir-containing oral antiviral regimen in chronic hepatitis C patients for the Damietta. Al-Azhar Assiut Med J. 2019; 17(1): 9–13, https://doi.org/10.4103/AZMJ.A....
7.
Halota W, Flisiak R, Boroń-Kaczmarska A, et al. Recommendations for the treatment of hepatitis C issued by the Polish Group of HCV Experts – 2016. J Clin Exp Hepatol. 2016; 2: 27–33. https://doi.org/10.5114/ceh.20....
8.
Stępień M, Rosińska M. Ogniska wirusowego zapalenia wątroby typu C w Polsce w latach 2003–2013. Procedury medyczne najczęstszą drogą przenoszenia zakażeń HCV. Przegl Epidemiol. 2015; 69(3): 585–590.
9.
Sakem B, Madaliński K, Nydegger U, et al. Hepatitis C virus epidemiology and prevention in Polish and Swiss population – similar and contrasting experiences. Ann Agric Environ Med. 2016; 23(3): 425–431. https://doi.org/10.5604/123219....
10.
Ziółkowski A, Błachnio A, Pąchalska M. Ocena zadowolenia z życia i zdrowia – Jakość życia seniorów. Ann Agric Environ Med. 2015; 22(1): 147–151. https://doi.org/10.5604/123219....
11.
Tomasiewicz K. Kiciak S, Murias-Bryłowska E. Współczesne poglądy na zagadnienie możliwości transmisji wirusa zapalenia wątroby typu C w placówkach opieki medycznej. Hepatology 2015; 15: 60–64. https://doi: 10.5114/hepatologia. 2015. 51781.
12.
Nguyen DB, Bixler D. Patel PR. Transmission of hepatitis C virus in the dialysis setting and strategies for its prevention. Semin Dial. 2019; 32(2): 127–134. https://doi.org/10.1111/sdi.12....
13.
Grabarczyk P, Medyńska J, Liszewski G, et al. HCV RNA and HIV RNA detection by Procleix HIV-1/ /HCV Assay in blood donors with various results of anti-HCV and anti-HIV EIA. J Transf Med. 2009; 1(1): 26–33.
14.
Cooke GS, Andrieus-Meyer I, Applegate TL, et al. Accelerating the elimination of viral hepatitis. Lancet Gastroenterol Hepatol. 2019; 4: 135–184. https://doi.org/10.1016/s2468-....
15.
Axley P, Ahmed Z, Ravi S, et al. Hepatitis C Virus and Hepatocellular Carcinoma: A Narrative Review. J Clin Transl Hepatol. 2018; 6: 79–84. https://doi.org/10.14218/JCTH.....
16.
Marinho RT, Barreira DP. Hepatitis C, stigma and cure. World J Gastroenterol. 2013; 19: 6703–6709. https://doi.org/10.3748/wjg.v1....
17.
Mui UN, Haley ChT, Tyring SK. Viral oncology: molecular biology and pathogenesis. J Clin Med. 2017; 6–12: 111. https://doi.org/10.3390/jcm612....
18.
Bosetti C, Turati F, La Vecchia C. Hepatocellular carcinoma epidemiology. Best Pract Res Clin Gastroenterol. 2014; 28(5): 753–770, https://doi.org/10.1016/j.bpg.....
19.
Muzica CM, Stanciu C, Anca Tri A, et al. Hepatocellular carcinoma after direct-acting antiviral hepatitis C virus therapy: A debate near the end. Word J Gastroenterol. 2020; 26(43): 6770–6781. https://doi.org/10.3748/wjg.v2....
20.
Sierpińska L. Narzędzia pomiaru jakości życia zakażonych wirusem HCV. J Educ Health Sport. 2017; 7(5): 185–196. http://dx.doi.org/10.5281/zeno....
21.
Felton BJ, Revension TA, Hionrichsen GA. (adaptacja Juczyński Z.). Skala akceptacji choroby AIS. In: Juczyński Z. Narzędzia pomiaru w promocji psychologii zdrowia. Warszawa: Pracownia Testów Psychologicznych; 2009. p. 162–166.
22.
Grochans E, Sychta D, Szkup M, reditor. Ocena relacji społecznych i środowiskowych pacjentów z przewlekłym wirusowym zapaleniem wątroby typu C. Probl Hig Epidemiol. 2010; 91(1): 131–136.
23.
Barański K, Szuba E, Olszanecka-Glinianowicz M, et al. Czynniki socjodemograficzne wpływające na poziom wiedzy dotyczącej dróg szerzenia się zakażenia w kontaktach niezwiązanych z procedurami medycznymi wśród pacjentów z WZW typu C. Ann Acad Med Siles. 2013; 67(5): 294–302.
24.
Zickmund S, Hillis SL, Barnett MJ, et al. Hepatitis C virus-infected patients report communications problems with physicians. Hepatology. 2004; 39(4): 999–1007. https://doi.org/10.1002/hep.20....
25.
El-Serag HB, Kanwal F, Richardson P, et al. Risk of hepatocellular carcinoma after sustained virological response in Veterans withhepatitis C virus infection. Hepatology. 2016; 64(1): 130–137. https://doi.org/10.1002/hep.28....
26.
Hoshida Y, Fuchs BC, Bardeesy N, et al. Pathogenesis and prevention of hepatitis C virus-induced hepatocellular carcinoma. J Hepatol. 2014; 61(1 Suppl): 79–90. https://doi.org/10.1016/j.jhep....
27.
Cardoso H, Silva M. Health-related quality of life in chronic hepatitis C. GE Port J Gastroenterol. 2017; 24(2): 55–57. https://doi.org/10.1159/000453....
28.
Barreira DP, Marinho RT, Bicho M, et al. Psychosocial and neurocognitive factors associated with hepatitis C – implications for future health and wellbeing. Front Psychol. 2018; 9(2666): 1–6. https://doi.org/10.3389/fpsyg.....
29.
Cardoso H, Silva M. Health-Related Quality of Life in Chronic Hepatitis C. GE Port 2017; 24(2): 55–57. https://doi.org/10.1159/000453....
30.
Cossais S, Schwarzinger M, Pol S, et al. Quality of life in patients with chronic hepatitis C infection: Severe comorbidities and disease perception matter more than liver-disease stage. PLoS One 3 May 2019; 14(5): e0215596. https://doi.org/10.1371/journa....
31.
Huang R, Rao H, Shang J, et al. A cross-sectional assessment of health-related quality of life in Chinese patients with chronic hepatitis c virus infection with EQ-5D. Health Qual Life Outcomes. 2018; 16(1): 124. https://doi.org/10.1186/s12955....
32.
López RH, Seiz AM, Portales MR, et al. Estudio de calidad de vida en pacient asasintomáticos con hepatitis C. Rev Esp Enferm Dig. 2020; 112(7): 520–524. https://doi.org/10.17235/reed.....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.