Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Neurodevelopmental outcome and early rehabilitation of premature babies – is it needed in the first 2 years of life?
1
Department of Rehabilitation and Physiotherapy, Medical University, Lublin, Poland
2
Department of Pediatric Rehabilitation, University Children’s Hospital, Lublin, Poland
3
Children Orthopaedic Department, Medical University, Lublin, Poland
4
Department of Biochemistry and Molecular Biology, Medical University, Lublin, Poland
5
Department of Anaesthesiological and Intensive Care Nursing, Medical University, Lublin, Poland
Corresponding author
Jolanta Taczała
Department of Rehabilitation and Physiotherapy, Medical University of Lublin, Poland, Prof. A. Gębali 2, 20-093, Lublon, Poland
Department of Rehabilitation and Physiotherapy, Medical University of Lublin, Poland, Prof. A. Gębali 2, 20-093, Lublon, Poland
Ann Agric Environ Med. 2021;28(1):172-178
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The aim of the study was to evaluate the neurodevelopmental outcomes of extremely premature babies at the age of 2 years, and to determine whether rehabilitation was carried out during this period. An additional aim was to determine the relationship between the use of rehabilitation and the degree of prematurity, asphyxia, birth weight, and the result of brain ultrasound.
Material and methods:
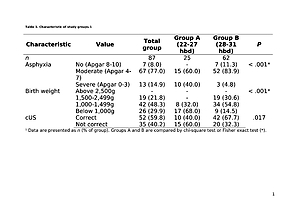
The study included 87 premature babies born between 24–31 weeks of pregnancy. A rehabilitation specialist assessed the neurodevelopmental outcomes of the children aged 2 years. Based on the documentation, the frequency of rehabilitation and its dependence on prematurity, asphyxia, birth weight and ultrasound results were analyzed.
Results:
Correct neurodevelopmental outcome in children aged 2 years was found in 57 (65%) children, of whom 40 (46%) did not undergo rehabilitation. Incorrect development was observed in a group of 30 children – 12 patients were diagnosed with CP (14%), and 18 (21%) had ‘red flags’ of development milestones, they underwent rehabilitation. There was no statistically significant relationship between the degree of prematurity, perinatal asphyxia, birth weight and rehabilitation in the first 2 years of life. Abnormal ultrasound results were more common in rehabilitated children (n = 25; 53%) than in children without rehabilitation (n = 10; 25%), p = 0.008.
Conclusions:
Correct neurodevelopmental outcome at the age of 2 reached two-thirds of extreme prematurities, most of which did not need rehabilitation during this period. According to the authors’ knowledge, this is the first study to show the percentage of premature babies who in the first 2 years of life did not require rehabilitation and achieved normal development.
The aim of the study was to evaluate the neurodevelopmental outcomes of extremely premature babies at the age of 2 years, and to determine whether rehabilitation was carried out during this period. An additional aim was to determine the relationship between the use of rehabilitation and the degree of prematurity, asphyxia, birth weight, and the result of brain ultrasound.
Material and methods:
The study included 87 premature babies born between 24–31 weeks of pregnancy. A rehabilitation specialist assessed the neurodevelopmental outcomes of the children aged 2 years. Based on the documentation, the frequency of rehabilitation and its dependence on prematurity, asphyxia, birth weight and ultrasound results were analyzed.
Results:
Correct neurodevelopmental outcome in children aged 2 years was found in 57 (65%) children, of whom 40 (46%) did not undergo rehabilitation. Incorrect development was observed in a group of 30 children – 12 patients were diagnosed with CP (14%), and 18 (21%) had ‘red flags’ of development milestones, they underwent rehabilitation. There was no statistically significant relationship between the degree of prematurity, perinatal asphyxia, birth weight and rehabilitation in the first 2 years of life. Abnormal ultrasound results were more common in rehabilitated children (n = 25; 53%) than in children without rehabilitation (n = 10; 25%), p = 0.008.
Conclusions:
Correct neurodevelopmental outcome at the age of 2 reached two-thirds of extreme prematurities, most of which did not need rehabilitation during this period. According to the authors’ knowledge, this is the first study to show the percentage of premature babies who in the first 2 years of life did not require rehabilitation and achieved normal development.
REFERENCES (53)
1.
Novak I, Morgan C, Adde L, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy Advances in Diagnosis and Treatment. JAMA Pediatr. 2017; 171(9): 897–907.
2.
Spittle AJ, Morgan C, Olsen JE, Novak I, Cheong JL. Early Diagnosis and Treatement of Cerebral Palsy in Children with a History of Preterm Birth. Clin Perinatol. 2018; 45(3): 409–420.
3.
Herskind A, Greisen G, Nielsen JB. Early identification and intervention in cerebral palsy. Dev Med Child Neurol. 2015 Jan; 57(1): 29–36.
4.
Bosanquet M, Copeland L, Ware R, Boyd R. A systematic review of tests to predict cerebral palsy in young children. Dev Med Child Neurol. 2013; 55: 418–26.
5.
Himpens E, Van den Broeck C, Calders P, Vanhaesebruck P. Prevalence, type, distribution and severity of cerebral palsy in relations to gestational age: a metaanalytic review. Dev Med Child Neurol. 2008 May; 50(5): 334–40.
6.
Platt MJ, Cans C, Johnson A, et al. Trends in cerebral palsy among infants of very low birthweight (<1500 g) or born prematurely (<32 weeks) in 16 European centres: a database study. Lancet 2007; 369: 43–50.
7.
Pelc K, Daniel I, Wenderickx B, Dan B. Primebrain group. Multicentre prospective randomised single-blind controlled study protocol of the effect of an additional parent-administered sensorimotor stimulation on neurological development of preterm infants: Primebrain. BMJ Open. 2017 Dec 3; 7(12).
8.
Tamis W. Pin a, Bev Eldridge b, Mary P. Galea: Motor trajectories from 4 to 18 months corrected age in infants born at less than 30 weeks of gestation. Early Hum Dev. 2010; 86: 573–580.
9.
Maitre NL, Slaughter JC, Aschner JL. Early prediction of cerebral palsy after neonatal intensive care using motor development trajectories in infancy. Early Hum Dev. 2013; 89: 781–6.
10.
Kułakowska Z. Some aspects of early diagnosis of brain lesions in newborn. Ped Pol. 2007; 82(10): 816–823.
11.
Hadders-Algra M. Early Diagnosis and Early Interwention i Cerebral Palsy. Frontiers in Neurology 2014.
12.
Cioni Giovanni, Inguaggiato Emanuela, Sgandurra Giuseppina. Early intervention in neurodevelopmental disorders: underlying neural mechanisms. Dev Med Child Neur. 2016; 58(Suppl. 4): 61–66.
13.
Hadders-Algra M. Early brain damage and the development of motor behavior in children: clues for therapeutic intervention? Neural Plast. 2001; 8: 31–49.
14.
Spittle A, Trevvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm, Semin Perinatol. 2016 Dec; 40(8): 542–548.
15.
White-Traut RC1, Rankin KM2, Yoder J3, Zawacki L4, Campbell S5, Kavanaugh K6, Brandon D7, Norr KF3. Relationship between mother-infant mutual dyadic responsiveness and premature infantdevelopment as measured by the Bayley III at 6 weeks corrected age. Early Hum Dev. 2018 Jun; 121: 21–26.
16.
Howe TH, Sheu CF, Wang TN, Hsu YW. Parenting stress in families with very low birth weight preterm infants in early infancy. Res Dev Disabil. 2014 Jul; 35(7): 1748–56.
17.
Hashkes PJ. Joint laxity is not equal to hypermobility in preterm born in children. J Ped. 2018; 197: 104–5.
18.
Duncan AF, Matthews MA. Neurodevelopmental Outcomes in Early Childhood. Clin Perinatol. 2018; 45: 377–392.
19.
Guzzetta A, Baldini S, Bancale A, et al. Massage accelerates brain development and the maturation of visual function. J Neurosci. 2009; 29: 6042–5.
20.
Linsell L, Malouf R, Marlow N, et al. Prognostic Factors for Poor Cognitive Development in Children Born Very Preterm or With Very Low Birth Weight: A Systematic Review. Jama Pediatrics 2015; 169(12): 1162–1172.
21.
Dosman CF, Andrews D, Goulden K. Evidence-based milestone ages as a framework for developmental surveillance. Paediatr Child Health 2012; 17: 561–568.
22.
Novak I, Hines M, Goldsmith S, et al. Clical prognostic messages from a systematic review on cerebral palsy. Pediatrics 2012; 130(5): 1285–312.
23.
Novak I, Mcintyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state with the evidence. Dev Med Child Neurol. 2013; 55: 885–910.
24.
Schandel D, Bhasin TK. Birth weight and gestational age characteristics of children with autism including a comparison with other developmental disabilities. Pediatrics 2008; 121: 1155–1164.
25.
Morgan C, Darrah J, Gordon AM, Harbourne R, Spittle A, Johnson R, Fetters L. Effectiveness of motor interventions in infants with cerebral palsy: a systematic review. Dev Med Chil Neur. 2016; 58: 900–909.
26.
Ferrari A. Cioni G. The Spastic Form of Cerebral Palsy. A Guide to the Assessement of Adaptive Functions. 2010, Springer-Verlag Italia, 31–50.
27.
Kilincaslan A, Mukaddes NM. Pervasive developmental disorders in individuals with cerebral palsy. Dev Med Child Neurol 2009; 51: 289–94.
28.
Einspieler C, Prechtl HF. Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment Retard Dev Disabil Res Rev. 2005; 11(1): 61–67.
29.
Einspieler C, Marschik PB, Bos AF, Ferrari F, Cioni G, Prechtl HF. Early markers for cerebral palsy: insights from the assessment of general movements. Future Neurol. 2012; 7: 709–717.
30.
Pierce K, Carter C, Weinfield M, et al. Detecting, studying, and treaning autism early: The one-year well-baby check-up approach. J Pediatr. 2011; 159: 458–465.
31.
Rutkowska M, Bekiesińska-Figatowska M, Kmita G, Terczyńska I, Polak K, Kalisiak M, Prażmowska D, Kiepura E, Szkudlińska-Pawlak S, Seroczyńska M, Helwich E. Neuroimaging results, short-term assessement of psychomotor development and the risk of autism spectrum disorder in extremly premature infants<28GA) – a prospective cohort study (preliminary report). Developmental Period Medicine 2018; XXII(1): 39–48.
32.
Younge N, Goldstein RF, Bann CM, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med. 2017; 376(7): 617–28.
33.
Moore T, Hennessy E, Myles J, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. BMJ 2012; 345: 1–15.
34.
Rysavy MA, Li L, Bell EF, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med. 2015; 372(19): 1801–11.
35.
Howe TH, Sheu CF, Wang TN, Hsu YW. Parenting stress in families with very low birth weight preterm infants in early infancy. Res Dev Disabil. 2014 Jul; 35(7): 1748–5.
36.
White-Traut RC, Rankin KM, Yoder J, Zawacki L, Campbell S, Kavanaugh K, Brandon D, Norr KF. Relationship between mother-infant mutual dyadic responsiveness and premature infantdevelopment as measured by the Bayley III at 6 weeks corrected age. Early Hum Dev. 2018 Jun; 121: 21–26.
37.
Palisano RJ, Chiarello LA, King GA, Novak I, Stoner T, Fiss A. Participation-based therapy for children with physical disabilities. Disabil Rehabil. 2012; 34: 1041–52.
38.
Chattopadthyay N, Mitra K. Neurodevelopmental outcome of high risk newborns discharged from special care baby units in a rural districts in India. J Public Health Res. 2015; 4: 318.
39.
Colver A, Fairhurst C, Pharoah P. Cerebral palsy. Lancet 2014; 383: 1240–49.
40.
Diwakar RK, Khurana O. Cranial Sonography in Preterm Infants with Short Review of Literature. J Pediatric Neurosci. 2018; 13(2): 141–149.
41.
Reid SM, Dagia CD, Ditchfield MR, Carlin JB, Reddihough DS. Population-based studies of brain imaging patterns in cerebral palsy. Dev Med Child Neurol. 2014; 56: 222–32.
42.
Muller-NC, Forcada-Guex M, Pierrehumbert B, et al. Prematurity, maternal stress and mother-child interactions. Early Hum Dev. 2004; 2: 145–158.
43.
Spittle A, Treyvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin Perinatol. 2016; 40(8): 542–8.
44.
Cong X, Wu J, Vittner D, Xu W, Hussain N, Galvin S, Fitzsimons M. The Impact of Cumulative Pain/Stress on Neurobehavioral Development of Preterm Infants in the NICU. Early Hum Dev. 2017 May; 108: 9–16.
45.
Als H, Duffy FH, McAnulty GB, Rivkin MJ, Vajapeyam S, Mulkern RV, Warfield SK, Huppi PS, Butler SC, Conneman N, et al. Early experience alters brain function and structure. Pediatrics, 2004 Apr; 113.
46.
Graven S, Browne JV. Sensory Development in the Fetus, Neonate, and Infant: Introduction and Overview. Newborn Infant Nurs Rev. 2008; 8(4): 169–172.
47.
Novak I, Thornton N, Morgan M, et al. Truth with hope: ethical challenges in disclosing „bad” diagnostic prognostic and intervention information. In: Rosenbaum P, Ronen GM, Racine E, et al. editors Ethic in child health: principles and cases in neurodisability. London MacKeith Press 2016.
48.
Baird G, McConachie H, Scrutton D. Parents’ perceptions of disclosure of the diagnosis of cerebral palsy. Arch Dis Child. 2000; 83(6): 475–80.
49.
Benzies KM, Magill-Evans JE, Hayden KA, et al. Key components of early intervention programs for preterm infants and their parents. A systematic reviews and meta-analysis. BMC Pregnancy Childbirth 2013; 13 (supl 1): 10.
50.
Aylward GP. Neurodevelopmental outcomes of infants born prematurely. J Dev Behav Pediatr. 2014; 35(6): 394–407.
51.
Joo JW, Choi JY, Rha DW, et al. Neuropsychological outcomes of preterm birth in children with no major neurodevelopmental impairments in early life. Ann Rehabil Med. 2015; 39(5): 676–85.
52.
Anderson PJ, Doyle LW. Cognitive and educational deficits in children born extremely preterm. Semin Perinatol. 2008; 32(1): 51–8.
53.
Di Rossa G, Cavallaro T, Alibrandi A, et al. Predictive role of milestones-related psychomotor profiles and long-term neurodevelopmental pitfalls in preterm infants. Early Human Develop. 2016; 101: 49–55.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.