Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Microbial contamination of money sorting facilities
1
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), Warsaw, Poland
2
Institute of Rural Health, Lublin, Poland
Corresponding author
Rafał L. Górny
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), ul. Czerniakowska 16, 00-701, Warsaw, Poland
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), ul. Czerniakowska 16, 00-701, Warsaw, Poland
Ann Agric Environ Med. 2021;28(1):61-71
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Money is the most common item with which we have daily contact. Circulated banknotes and coins can become microbiologically contaminated and act as both a source and a means of spreading such pollutants.
Material and methods:
The study was carried out in three money sorting facilities in Poland. Bioaerosol samples were collected using a 6-stage Andersen impactor, and microorganisms deposited on tabletop surfaces were sampled using the swab method. Bacterial and fungal concentrations were calculated and all isolated species were taxonomically identified.
Results:
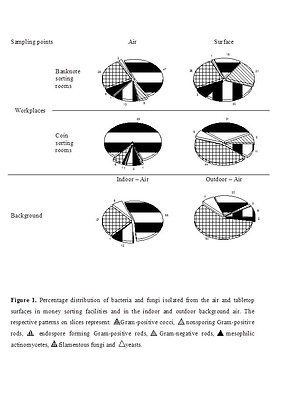
The study confirmed that means of payment are active sources of microbial emission in money sorting facilities. The bioaerosol concentrations did not exceed the threshold limit values proposed for this type of office premises. It confirms that ventilation systems in these facilities worked efficiently, protecting them from the migration of microbial contaminants present in both indoor and outdoor (atmospheric) background air. On the other hand, the average concentrations of bacteria and fungi on tabletop surfaces in banknote and coin sorting rooms were above the proposed purity levels for indoor surfaces and should be treated as microbiologically contaminated. Microbiota isolated from the air and surfaces were very diverse and among those strains were bacterial and fungal pathogens that can pose a health threat to exposed individuals.
Conclusions:
The results showed that employees in money sorting facilities were exposed to microorganisms that may contribute to the development of adverse health outcomes. To protect them, highly efficient hygienic measures should be introduced in this working environment, to prevent both unwanted pollution and subsequent secondary emission of microbial contaminants from sorted means of payment and tabletop surfaces.
Money is the most common item with which we have daily contact. Circulated banknotes and coins can become microbiologically contaminated and act as both a source and a means of spreading such pollutants.
Material and methods:
The study was carried out in three money sorting facilities in Poland. Bioaerosol samples were collected using a 6-stage Andersen impactor, and microorganisms deposited on tabletop surfaces were sampled using the swab method. Bacterial and fungal concentrations were calculated and all isolated species were taxonomically identified.
Results:
The study confirmed that means of payment are active sources of microbial emission in money sorting facilities. The bioaerosol concentrations did not exceed the threshold limit values proposed for this type of office premises. It confirms that ventilation systems in these facilities worked efficiently, protecting them from the migration of microbial contaminants present in both indoor and outdoor (atmospheric) background air. On the other hand, the average concentrations of bacteria and fungi on tabletop surfaces in banknote and coin sorting rooms were above the proposed purity levels for indoor surfaces and should be treated as microbiologically contaminated. Microbiota isolated from the air and surfaces were very diverse and among those strains were bacterial and fungal pathogens that can pose a health threat to exposed individuals.
Conclusions:
The results showed that employees in money sorting facilities were exposed to microorganisms that may contribute to the development of adverse health outcomes. To protect them, highly efficient hygienic measures should be introduced in this working environment, to prevent both unwanted pollution and subsequent secondary emission of microbial contaminants from sorted means of payment and tabletop surfaces.
Górny RL, Gołofit-Szymczak M, Wójcik-Fatla A, Cyprowski M, Stobnicka-Kupiec A, Ławniczek-Wałczyk A. Microbial contamination of money sorting facilities. Ann Agric Environ Med.doi: 10.26444/aaem/132321
REFERENCES (68)
1.
Abrams BL, Waterman NG. Dirty money. J Am Med Assoc. 1972; 219: 1202–1203. https://doi.org/10.1001/jama.2....
2.
Badvi JA, Jawed K, Jawed M. Lower denomination and dirty currency carries more contaminated than higher denomination in Pakistan. Int J Vaccines Vaccination. 2017; 4(3): 1–8. https://doi.org/10.15406/ijvv.....
3.
Ahmed MSU, Parveen S, Nasreen T, et al. Evaluation of the microbial contamination of Bangladesh paper currency notes (Taka) in circulation. Adv Biol Res. 2010; 4: 266–271.
4.
Ukwuru M, Gabriel A. Cross contamination between food and money due to simultaneous handling. J Appl Sci Environ. 2012; 3: 42–48.
5.
Badvi JA, Hafiz S, Baloch L, et al. Various outlets are the potential source of bacterial infections through the Pakistan currency notes. Med Channel. 2013; 19: 87–92.
6.
Sharma S, Sumbali G. Contaminated money in circulation: a review. Int J Rec Sci Res. 2014; 5(9): 1533–1540.
7.
Butt A, Malik S. Microbial and parasitic contamination on circulating Pakistani currency. Adv Life Sci. 2015; 2(4): 150–157
8.
Gedik H, Voss TA, Voss A. Money and transmission of bacteria. Antimicrob Resist Infect Control. 2013; 2: 22. https://doi.org/10.1186/2047-2....
9.
Angelakis E, Azhar EI, Bibi F, et al. Paper money and coins as potential vectors of transmissible disease. Future Microbiol. 2014; 9: 249–261. https://doi.org/10.2217/fmb.13....
10.
Elemam MM, Dhawi A, Ben Shaban M, et al. A study of bacterial contamination on Libyan banknotes in circulation. Am J Microbiol Biotechnol. 2016; 3: 1–6.
11.
Sucilathangam G, Reventh AM, Valvizhi G, et al. Assessment of microbial contamination of paper currency notes in circulation. Int J Current Microbiol Appl Sci. 2016; 5: 735–741. https://doi.org/10.20546/ijcma....
12.
Girma G. Health risk associated with handling of contaminated paper currencies in circulation: a review. J Food Nutr Sci. 2015; 2: 49–54. https://doi.org/10.15436/2377-....
13.
Lo Sia Su G, Coden C, Cruz A, et al. Bacteriological and parasitological assessment of currencies obtained in selected markets of Metro Manila. Asian Pac J Trop Dis. 2015; 5: 468–470. https://doi.org/10.1016/s2222-....
14.
Motteran F. Microbial contamination of currency. Int J Health Life Sci. 2018; 4: e79609. https://doi.org/10.5812/ijhls....
15.
Neel GR, Marcelline U, Izere C, et al. Contamination of currency notes and coins as source of transmissible diseases. Int J Pharm Res Health Sci. 2018; 6: 2334–2337.
16.
Khin NO, Phyu PW, Aung MB, et al. Contamination of currency notes with enteric bacterial pathogens. J Diarrhoeal Dis Res. 1989; 7: 92–94.
17.
Uraku AJ, Obaji PI, Nworie B. Potential risk of handling Nigerian currency notes. Int J Adv Biol Res. 2012; 2: 228–233.
18.
Pope TW, Ender PT, Woelk WK, et al. Bacterial contamination of paper currency. Southern Med J. 2002; 95: 1406–1410. https://doi.org/10.1097/000076....
19.
Vriesekoop F, Chen J, Oldaker J, et al. Dirty money: a matter of bacterial survival, adherence, and toxicity. Microorganisms. 2016; 4: 42. https://doi.org/10.3390/microo....
20.
Amirabad LM, Jonoobi M, Mousavi NS, et al. Improved antifungal activity and stability of chitosan nanofibers using cellulose nanocrystal on banknote papers. Carbohyd Polym. 2018; 189: 229–237. https://doi.org/10.1016/j.carb...
21.
Zarayneh S, Sepahi AA, Janoobi M, et al. Comparative antibacterial effects of cellulose nanofiber, chitosan nanofiber, chitosan/cellulose combination and chitosan alone against bacterial contamination of Iranian banknotes. Int J Biol Macromol. 2018; 118: 1045–1054. https://doi.org/10.1016/j.ijbi....
22.
Sharma V, Sumbali G. Diversity of cellulose active micromycetes in the ant-hill soil environment of parks and gardens of Jammu city (India). Int J Pharm Bio Sci. 2013; 4: 541–548.
23.
Riddell S, Goldie S, Hill A, et al. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol J. 2020; 17: 145. https://doi.org/10.1186/s12985....
24.
Jalali S, Kohli S, Latka C, et al. Screening currency notes for microbial pathogens and antibiotic resistance genes using a shotgun metagenomic approach. PLoS ONE. 2015; 10: e0128711. https://doi.org/10.1371/journa....
25.
Pereira de Fonseca T, Pessoa R, Sanabani SS. Molecular analysis of bacterial microbiota on Brazilian currency notes surfaces. Int J Environ Res Pub Health. 2015; 12: 13276–13288. https://doi.org/10.3390/ijerph....
26.
Hassan M, Honua M. The hygienic and microbial status of Sudanese banknotes, Khartoum state, Sudan. Int J Community Med Pub Health. 2017; 4: 923–9.
27.
https://doi.org/10.18203/2394-... AMA, Alhussaini MS, Al-Ghanayem AA, et al. Isolation and identification of pathogenic bacteria and fungi from some Saudi bank note currency. Biosci Biotechnol Res Asia. 2017; 14: 715–720. https://doi.org/10.13005/bbra/....
28.
Abirami B, Kumar T, Saravanamuthu R. Studies on the fungal flora of Indian currency. Asian J Res Pharm Sci. 2012; 2: 33–36.
29.
Snehalatha V, Malashree R, Soni P. Isolation, enumeration and antimicrobial susceptibility of predominant microbes associated with currency notes. Int J Curr Microbiol Appl Sci. 2016; 5(8): 650–657. https://doi.org/10.20546/ijcma....
30.
Jiang X, Doyle MP. Fate of Escherichia coli O157:H7 and Salmonella enteritidis on currency. J Food Protect. 1999; 62: 805–807. https://doi.org/10.4315/0362-0....
31.
Kuria JK, Wahome RG, Jobalamin M, et al. Profile of bacteria and fungi on money coins. East Afr Med J. 2009; 86(4): 151–155. https://doi.org/10.4314/eamj.v....
32.
Thiruvengadam S, Shreenidhi KS, Vidhyalakshmi H, et al. A study of bacterial profiling on coins and currencies under circulation and identifying the virulence gene in Chennai (TN). Int J ChemTech Res. 2014; 6(9): 4108–4114.
33.
Varusha SC, Sethu G. Paper money and coins as potential vectors in transmissible diseases – a review. J Pharm Sci Res. 2017; 9(2): 139–141.
34.
Enemuor SC, Victor PI, Oguntibeju OO. Microbial contamination of currency counting machines and counting room environment in selected commercial banks. Sci Res Essays. 2012; 71: 508–511. https://doi.org/10.5897/sre11.....
35.
Murray PR, Rosenthal KS, Pfaller MA. Medical microbiology, 7th ed. Philadelphia: Elsevier Saunders; 2013.
36.
Litwinow MA. Opriedielitiel mikroskopiczeskich po¬czwiennych gribow. Leningrad: Izdatielstwo Nauka; 1967.
37.
Domsch KH, Gams W, Anderson TH. Compendium of soil fungi. Eching: IHV Verlag; 1993.
38.
Klich MA. Identification of common Aspergillus species. Utrecht: Centraalbureau voor Schimmelcultures; 2002.
39.
Samson RA, Hoekstra ES, Frisvad JC. Introduction to food- and airborne fungi. 7th ed. Utrecht: Centraalbure¬au voor Schimmelcultures; 2004.
40.
St-Germain G, Summerbell R. Identifying Fungi: a Clinical Laboratory Handbook, 2nd ed. Belmont: Star Publishing Company; 2011.
41.
Bosshard PP, Zbinden R, Abels S, et al. 16S rRNA gene sequencing versus the API 20 NE system and the VITEK 2 ID-GNB card for identification of nonfermenting gram-negative bacteria in the clinical laboratory. J Clin Microbiol. 2006; 44: 1359–1366. https://doi.org/10.1128/jcm.44....
42.
Frank JA, Reich CI, Sharma S, et al. Critical evaluation of two primers commonly used for amplification of bacterial 16S rRNA genes. Appl Environ Microbiol. 2008; 74: 2461–2470. https://doi.org/10.1128/aem.02....
43.
White TJ, Bruns T, Lee S, et al. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In: Innins MA, Gelf DH, Sninsky JJ, White TJ, editors. PCR Protocols. A Guide to Methods and Applications. San Diego: Academic Press Inc.; 1990. p. 315–322.https://doi.org/10.1016/b978-0....
44.
Brandys RC, Brandys GM. Worldwide exposure standards for mold and bacteria. 10th ed. Hinsdale: OEHCS Inc., Publications Division; 2012.
45.
Górny RL, Dutkiewicz J. Bacterial and fungal aerosols in indoor environment in Central and Eastern European countries. Ann Agric Environ Med 2002; 9: 17–23.
46.
Górny RL. Harmful biological agents. In: Pośniak M, editor. Harmful Agents in the Working Environment–Admissible Values 2018. Warsaw: Central Institute for Labour Protection–National Research Institute; 2018. p. 149–157.
47.
Commission Directive (EU) 2019/1833 of 24 October 2019 amending Annexes I, III, V and VI to Directive 2000/54/EC of the European Parliament and of the Council as regards purely technical adjustments. OJ L. 2019; 279: 54–79.
48.
Ordinance of the Minister of Health of April 22, 2005, on hazardous biological agents in the work environment and the protection of health of workers occupationally exposed to them: Law Gazette 2005; 48(288/5): 421–439.
49.
Yates MV, Nakatsu CK, Miller RV, Pillai SD, editors. Manual of Environmental Microbiology. 4th ed. Washington, DC: ASM Press; 2016.
50.
Adan OCG, Samson RA, editors. Fundamentals of mold growth in indoor environments and strategies for healthy living. Wageningen: Wageningen Academic Publishers, 2011.
51.
Harkawy A, Górny RL, Ogierman L, et al. Bioaerosol assessment in naturally ventilated historical library building with restricted personnel access. Ann Agric Environ Med. 2011; 18: 323–329.
52.
Górny RL, Harkawy AS, Ławniczek-Wałczyk A, et al. Exposure to culturable and total microbial particles in cultural heritage conservation laboratories. Ann Agric Environ Med. 2015; 22(1): 18–28. https://doi.org/10.13075/ijome....
53.
Chełkowski J. 2010. Mikotoksyny, grzyby toksynotwórcze i miko-toksykozy. http://www.cropnet.pl/dbases/m... (access: 2020.11.12).
54.
Dutkiewicz J, Śpiewak R, Jabłoński L, Szymańska J. Occupational biohazards. Classification, exposed workers, measurements, prevention. Lublin: Ad Punctum; 2007.
55.
Kemp P, Neumeister-Kemp H. Australian mould guideline. Osborne Park: The Enviro Trust, 2010.56.
56.
Elsharief ME, Haider JS, Waly S. A study of bacterial contamination of paper currency notes circulating in Zliten area and their antibiotic resistance. J Human Appl Sci. 2018; 31: 99–115.
57.
Schuster E, Dunn-Coleman N, Frisvad JC, et al. On the safety of Aspergillus niger: A review. Appl Microbiol Biotechnol. 2002; 59: 426–435. https://doi.org/10.1007/s00253....
58.
Ozcan M, Ozcan MK. Karaarslan A, et al. Concomitant otomycosis and dermatomycoses: a clinical and microbiological study. Eur Arch Otorhinolaryngol. 2003; 260: 24–27. https://doi.org/10.1007/s00405....
59.
Ozhak-Baysan B, Alastruey-Izquierdo A, Saba R. Aspergillus alliaceus and Aspergillus flavus co-infection in an acute myeloid leukemia patient. J Med Mycol. 2010; 48: 995–999. https://doi.org/10.3109/136937....
60.
Campbell MC, Steward JK. Handbook of medical mycology. New York: Wiley Medical Publisher; 1980. p. 229–239.
61.
Ekenna O, Uba A, Chikwem JO, et al. Relevance of moldy fungi as agents of chronic lower respiratory tract infection in patients seen in Maiduguri, Nigeria. West Afr J Med. 2007; 26: 117–120.
62.
Antoniadou A. Outbreaks of zygomycosis in hospitals. Clin Microbiol Infect. 2009; 5: 55–59. https://doi.org/10.1111/j.1469....
63.
Zhang N, O’Donnell K, Sutton DA, et al. Members of the Fusarium solani species complex that cause infections in both humans and plants are common in the environment. J Clin Microbiol. 2006; 44: 2186–2190. https://doi.org/10.1128/jcm.00....
64.
Halawa A, Henry PD, Sarrubi FA. Candida endocarditis associated with cardiac rhythm management devices: Review with current treatment guidelines. Mycoses. 2011; 54: 168–174. https://doi.org/10.1111/j.1439....
65.
Madhavan P, Jamal F, Chong PP. Laboratory isolation and identification of Candida species. J Appl Sci. 2011; 11: 2870–2877. https://doi.org/10.3923/jas.20....
66.
Currie BP, Casadevall A. Estimation of the prevalence of cryptococcal infection among patients infected with the human immunodeficiency virus in New York City. Clin Infect Dis. 1994; 19: 1029–1033. https://doi.org/10.1093/clinid....
67.
Michaels B. Handling money and serving ready-to-eat food. Food Service Technol. 2002; 2(1): 1–3. https://doi.org/10.1046/j.1471...
68.
Poszytek K. Microbial cellulose utilization. Post Mikrobiol. 2016; 55(2): 132–146.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.