Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
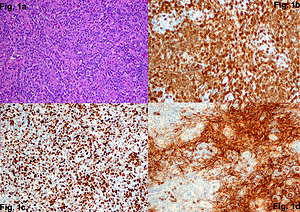
Fever, rash, and eosinophilia – early signs of angioimmunoblastic T-cell lymphoma
1
Chair and Department of Dermatology, Venerology and Paediatric Dermatology, Faculty of Medicine, Medical University, Lublin, Poland
2
Chair and Department of Internal Diseases, Faculty of Medicine, Medical University, Lublin, Poland
3
Chair and Department of Clinical Pathomorphology, Faculty of Medicine, Medical University, Lublin, Poland
4
Department of Internal Diseases and Hypertension, Institute of Rural Health, Lublin, Poland
Corresponding author
Bartłomiej Wawrzycki
Chair and Department of Dermatology, Venerology and Paediatric Dermatology. Faculty of Medicine. Medical university of Lublin., Lublin. ul. Staszica 14, 20-080, Lublin, Poland
Chair and Department of Dermatology, Venerology and Paediatric Dermatology. Faculty of Medicine. Medical university of Lublin., Lublin. ul. Staszica 14, 20-080, Lublin, Poland
Ann Agric Environ Med. 2021;28(3):525-530
KEYWORDS
lymphomaeosinophiliarashfeverimmunoblastic lymphadenopathyhypereosinophilic syndromenon-Hodgkinexanthema
TOPICS
ABSTRACT
Angioimmunoblastic T-cell lymphoma (AITL) is an uncommon lymphoma of elderly adults with a poor prognosis. AITL patients show systemic symptoms, lymphadenopathy, and not infrequently, skin rash with various dysimmune phenomena rashes. The case is presented of a 68-year-old male with skin rash, lymphadenopathy and hypereosinophilia who, after investigations, was diagnosed with AITL. Despite the treatment used, the patient’s condition gradually deteriorated and died due to heart and kidney failure. The diagnosis of AITL is often established only after several weeks or months because of transient physical findings, non-specific symptoms, and a broad range of serologic or radiologic abnormalities. Some patients with AITL experience non-specific dermatitis and eosinophilia. The presented case should raise awareness of the
presentations of AITL which is important for physicians to reach an accurate diagnosis.
REFERENCES (39)
1.
Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016; 127(20): 2375–90. doi: 10.1182/blood-2016-01-643569.
2.
Lunning MA, Vose JM. Angioimmunoblastic T-cell lymphoma: the many-faced lymphoma. Blood. 2017; 129(9): 1095–1102. doi: 10.1182/blood-2016-09-692541.
3.
Federico M, Rudiger T, Bellei M, et al. Clinicopathologic characteristics of angioimmunoblastic T-cell lymphoma: analysis of the international peripheral T-cell lymphoma project. J Clin Oncol. 2013; 31(2): 240–6. doi: 10.1200/JCO.2011.37.3647.
4.
Ermann DA, Vardell VA, Silberstein PT. Angioimmunoblastic T-Cell Lymphoma: Patient Characteristics and Survival Outcomes. Blood. 2019; 134(Supplement_1): 2194–2194. doi: 10.1182/blood-2019-132077.
5.
Xu B, Liu P. No survival improvement for patients with angio immuno-blastic T-cell lymphoma over the past two decades: a population-based study of 1207 cases. PLoS One. 2014; 9(3): e92585. doi: 10.1371/journal.pone.0092585.
6.
Lachenal F, Berger F, Ghesquieres H, et al. Angioimmunoblastic T-cell lymphoma: clinical and laboratory features at diagnosis in 77 patients. Medicine (Baltimore). 2007; 86(5): 282–292. doi: 10.1097/MD.0b013e3181573059.
7.
de Leval L, Gisselbrecht C, Gaulard P. Advances in the understanding and management of angioimmunoblastic T-cell lymphoma. Br J Haematol. 2010; 148(5): 673–89. doi: 10.1111/j.1365-2141.2009.08003.x.
8.
de Leval L, Parrens M, Le Bras F, et al. Angioimmunoblastic T-cell lymphoma is the most common T-cell lymphoma in two distinct French information data sets. Haematologica. 2015; 100(9): e361–4. doi: 10.3324/haematol.2015.126300.
9.
Broccoli A, Zinzani PL. Angioimmunoblastic T-Cell Lymphoma. Hematol Oncol Clin North Am. 2017; 31(2): 223–238. doi: 10.1016/j.hoc.2016.12.001.
10.
Ohsaka A, Saito K, Sakai T, et al. Clinicopathologic and therapeutic aspects of angioimmunoblastic lymphadenopathy-related lesions. Cancer. 1992; 69(5): 1259–67. doi: 10.1002/cncr.2820690531.
11.
Chernova NG, Soboleva NP, Mariina SA, et al. Immunoglobulinopathies in patients with angioimmunoblastic T-cell lymphoma. Ter Arkh. 2018; 90(7): 51–56. doi: 10.26442/terarkh201890751-56.
12.
Zhang Y, Lee D, Brimer T, Hussaini M, Sokol L. Genomics of Peripheral T-Cell Lymphoma and Its Implications for Personalized Medicine. Mini Review. Front Oncol. 2020; 10(898): 898. doi: 10.3389/fonc.2020.00898.
13.
Yao Y, Chen CL, Yu D, Liu Z. Roles of follicular helper and regulatory T cells in allergic diseases and allergen immunotherapy. Allergy. 2021; 76(2): 456–470. doi: 10.1111/all.14639.
14.
Chiba S, Sakata-Yanagimoto M. Advances in understanding of angioimmunoblastic T-cell lymphoma. Leukemia. 2020; 34(10): 2592–2606. doi: 10.1038/s41375-020-0990-y.
15.
Botros N, Cerroni L, Shawwa A, et al. Cutaneous manifestations of angioimmunoblastic T-cell lymphoma: clinical and pathological characteristics. Am J Dermatopathol. 2015; 37(4): 274–83. doi: 10.1097/DAD.0000000000000144.
16.
Martel P, Laroche L, Courville P, et al. Cutaneous involvement in patients with angioimmunoblastic lymphadenopathy with dysproteinemia: a clinical, immunohistological, and molecular analysis. Arch Dermatol. 2000; 136(7): 881–6. doi: 10.1001/archderm.136.7.881.
17.
Lee WJ, Won KH, Choi JW, et al. Cutaneous angioimmunoblastic T-cell lymphoma: Epstein-Barr virus positivity and its effects on clinicopathologic features. J Am Acad Dermatol. 2019; 81(4): 989–997. doi: 10.1016/j.jaad.2018.08.053.
18.
Oishi N, Sartori-Valinotti JC, Bennani NN, et al. Cutaneous lesions of angioimmunoblastic T-cell lymphoma: Clinical, pathological, and immunophenotypic features. J Cutan Pathol. 2019; 46(9): 637–644. doi: 10.1111/cup.13475.
19.
Archimbaud E, Coiffier B, Bryon PA, Vasselon C, Brizard CP, Viala JJ. Prognostic factors in angioimmunoblastic lymphadenopathy. Cancer. 1987; 59(2): 208–12. doi: 10.1002/1097-0142(19870115)59:2<208::aid-cncr2820590205>3.0.co;2-7.
20.
Siegert W, Nerl C, Agthe A, et al. Angioimmunoblastic lympha-denopathy (AILD)-type T-cell lymphoma: prognostic impact of clinical observations and laboratory findings at presentation. The Kiel Lymphoma Study Group. Ann Oncol. 1995; 6(7): 659–64. doi: 10.1093/oxfordjournals.annonc.a059281.
21.
Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013; 68(5): 693 e1–14; quiz 706–8. doi: 10.1016/j.jaad.2013.01.033.
22.
Kardaun SH. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS). In: Shear NH, Dodiuk-Gad RP, eds. Advances in Diagnosis and Management of Cutaneous Adverse Drug Reactions. Springer Singapore; 2019: 87–104: chap Chapter 7.
23.
Jeong J, Sim DW, Yu JE, et al. Differentiation of angioimmunoblastic T-cell lymphoma from DRESS syndrome. J Allergy Clin Immunol Pract. 2019; 7(5): 1684–1686 e1. doi: 10.1016/j.jaip.2018.11.048.
24.
Werbel T, Castrovinci P, Contestable J. Ethosuximide-induced drug reaction with eosinophilia and systemic symptoms with mediastinal lymphadenopathy. Pediatr Dermatol. 2019; 36(4): e99-e101. doi: 10.1111/pde.13848.
25.
Eng V, Kulkarni SK, Kaplan MS, Samant SA, Sheikh J. Hypereosinophilia with angioimmunoblastic T-cell lymphoma. Ann Allergy Asthma Immunol. 2020; 124(5): 513–515. doi: 10.1016/j.anai.2020.01.028.
26.
Hsieh FH. Hypereosinophilic syndrome. Ann Allergy Asthma Immunol. 2014; 112(6): 484–8. doi: 10.1016/j.anai.2014.03.004.
27.
Khoury P. Lymphocytic-Variant Hypereosinophilic Syndromes. Hematologist. 2017; 14(6). doi: 10.1182/hem.V14.6.7884.
28.
Ogbogu PU, Bochner BS, Butterfield JH, et al. Hypereosinophilic syndrome: a multicenter, retrospective analysis of clinical characteristics and response to therapy. J Allergy Clin Immunol. 2009; 124(6): 1319–25 e3. doi: 10.1016/j.jaci.2009.09.022.
29.
King RL, Tan B, Craig FE, et al. Reactive Eosinophil Proliferations in Tissue and the Lymphocytic Variant of Hypereosinophilic Syndrome. Am J Clin Pathol. 2021; 155(2): 211–238. doi: 10.1093/ajcp/aqaa227.
30.
Marzano AV, Genovese G. Eosinophilic Dermatoses: Recognition and Management. Am J Clin Dermatol. 2020; 21(4): 525–539. doi: 10.1007/s40257-020-00520-4.
31.
Sade K, Mysels A, Levo Y, Kivity S. Eosinophilia: A study of 100 hospitalized patients. Eur J Intern Med. 2007; 18(3): 196–201. doi: 10.1016/j.ejim.2006.09.031.
32.
Thompson Coon J, Pittler M, Ernst E. Herb-drug interactions: survey of leading pharmaceutical/herbal companies. Arch Intern Med. 2003; 163(11): 1371. doi: 10.1001/archinte.163.11.1371-a.
33.
Peju M, Deroux A, Pelloux H, Bouillet L, Epaulard O. Hypereosinophilia: Biological investigations and etiologies in a French metropolitan university hospital, and proposed approach for diagnostic evaluation. PLoS One. 2018; 13(9): e0204468. doi: 10.1371/journal.pone.0204468.
34.
Klion AD. How I treat hypereosinophilic syndromes. Blood. 2015; 126(9): 1069–77. doi: 10.1182/blood-2014-11-551614.
35.
Wang SA. The Diagnostic Work-Up of Hypereosinophilia. Pathobiology. 2019; 86(1): 39–52. doi: 10.1159/000489341.
36.
Jin JJ, Butterfield JH, Weiler CR. Hematologic Malignancies Identified in Patients with Hypereosinophilia and Hypereosinophilic Syndromes. J Allergy Clin Immunol Pract. 2015; 3(6): 920–5. doi: 10.1016/j.jaip.2015.06.009.
37.
Shomali W, Gotlib J. World Health Organization-defined eosinophilic disorders: 2019 update on diagnosis, risk stratification, and management. Am J Hematol. 2019; 94(10): 1149–1167. doi: 10.1002/ajh.25617.
38.
Andersen CL, Siersma VD, Hasselbalch HC, et al. Eosinophilia in routine blood samples and the subsequent risk of hematological malignancies and death. Am J Hematol. 2013; 88(10): 843–7. doi: 10.1002/ajh.23515.
39.
Khoury P, Bochner BS. Consultation for Elevated Blood Eosinophils: Clinical Presentations, High Value Diagnostic Tests, and Treatment Options. J Allergy Clin Immunol Pract. 2018; 6(5): 1446–1453. doi: 10.1016/j.jaip.2018.04.030.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.