Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Diagnostic and therapeutic approach to children with Nijmegen breakage syndrome in relation to development of lymphoid malignancies
1
Department of Paediatric Haematology, Oncology, and Transplantology, Medical University, Lublin, Poland
2
Laboratory of Genetic Diagnostics, Department of Paediatric Haematology, Oncology and Transplantology, Medical University, Lublin, Poland
Corresponding author
Aleksandra Filipiuk
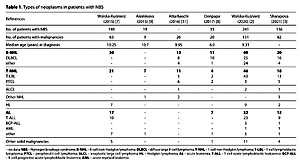
Medical University of Lublin, Department of Pediatric Hematology, Oncology, and Transplantology, A. Gębali, 20-093, Lublin, Poland
Medical University of Lublin, Department of Pediatric Hematology, Oncology, and Transplantology, A. Gębali, 20-093, Lublin, Poland
Ann Agric Environ Med. 2022;29(2):207-214
KEYWORDS
diagnosislymphomaantineoplastic agentsNijmegen Breakage SyndromeleukemiaHaematopoietic Stem Cell Transplantation
TOPICS
ABSTRACT
Introduction and objective:
Nijmegen breakage syndrome (NBS) is a rare chromosomal instability disorder. The majority of patients carry founder mutation in the NBN gene (c.657_661del5). Characteristic features of the NBS include progressive microcephaly, dysmorphic facial features, immunodeficiency, and high predisposition to malignancy with cumulative cancer incidence by the age of 20 years, and amounted to over 70%. The aim of study is to present the latest methods of diagnosis, potential cancer risk factors and treatment of lymphoid malignancies in children with NBS.
Review methods:
To review the evidence using PubMed and Google Scholar search which included articles published between 2009–2021, focusing on articles published between 2013–2021.
Abbreviated description of the state of knowledge:
The average delay in diagnosis of NBS ranges from 4–5 years. Neonatal screening of T-cell excision circles (TRECs) and kappa-deleting recombination excision circles (KRECs) seems favourable in NBS. There are no specific protocols for the treatment of lymphoid malignancies in children with NBS, and full- dose chemotherapy is the most frequently applied method. Reducing the doses of chemotherapy does not significantly reduce the toxicity. Main cause of death is cancer progression and treatment-related mortality mostly associated with infectious complications. Patients with diagnosed cancer who received haematopoietic stem cell transplantation (HSCT) had significantly higher 20-year OS than those who did not (42.7% vs. 30.3%).
Summary:
Further meta-analysis is essential to establish the best monitoring and treatment regimen in patients with NBS and lymphoid malignancies.
Nijmegen breakage syndrome (NBS) is a rare chromosomal instability disorder. The majority of patients carry founder mutation in the NBN gene (c.657_661del5). Characteristic features of the NBS include progressive microcephaly, dysmorphic facial features, immunodeficiency, and high predisposition to malignancy with cumulative cancer incidence by the age of 20 years, and amounted to over 70%. The aim of study is to present the latest methods of diagnosis, potential cancer risk factors and treatment of lymphoid malignancies in children with NBS.
Review methods:
To review the evidence using PubMed and Google Scholar search which included articles published between 2009–2021, focusing on articles published between 2013–2021.
Abbreviated description of the state of knowledge:
The average delay in diagnosis of NBS ranges from 4–5 years. Neonatal screening of T-cell excision circles (TRECs) and kappa-deleting recombination excision circles (KRECs) seems favourable in NBS. There are no specific protocols for the treatment of lymphoid malignancies in children with NBS, and full- dose chemotherapy is the most frequently applied method. Reducing the doses of chemotherapy does not significantly reduce the toxicity. Main cause of death is cancer progression and treatment-related mortality mostly associated with infectious complications. Patients with diagnosed cancer who received haematopoietic stem cell transplantation (HSCT) had significantly higher 20-year OS than those who did not (42.7% vs. 30.3%).
Summary:
Further meta-analysis is essential to establish the best monitoring and treatment regimen in patients with NBS and lymphoid malignancies.
REFERENCES (58)
1.
Seemanova E, Varon R, Vejvalka J, et al. The Slavic NBN Founder Mutation: A Role for Reproductive Fitness?. PLoS One. 2016; 11(12): e0167984. https://doi.org/10.1371/journa....
2.
Wolska-Kusnierz B, Pastorczak A, Fendler W, et al. Hematopoietic Stem Cell Transplantation Positively Affects the Natural History of Cancer in Nijmegen Breakage Syndrome. Clin Cancer Res. 2021; 27(2): 575–584. https://doi.org/10.1158/1078-0....
3.
Sharapova SO, Pashchenko OE, Bondarenko AV, et al. Geographical Distribution, Incidence, Malignancies, and Outcome of 136 Eastern Slavic Patients With Nijmegen Breakage Syndrome and NBN Founder Variant c.657_661del5. Front Immunol. 2021; 11: 602482. https://doi.org/10.3389/fimmu.....
4.
Chrzanowska KH, Gregorek H, Dembowska-Bagińska B, Kalina MA, Digweed M. Nijmegen breakage syndrome (NBS). Orphanet J Rare Dis. 2012; 7: 13. https://doi.org/10.1186/1750-1....
5.
Meijers RWJ, Dzierzanowska-Fangrat K, Zborowska M, et al. Circulating T Cells of Patients with Nijmegen Breakage Syndrome Show Signs of Senescence [published correction appears in J Clin Immunol. 2018 Apr 23]. J Clin Immunol. 2017; 37(2): 133–142. https://doi.org/10.1007/s10875....
6.
Piatosa B, Wolska-Kuśnierz B, Tkaczyk K, et al. T Lymphocytes in Patients With Nijmegen Breakage Syndrome Demonstrate Features of Exhaustion and Senescence in Flow Cytometric Evaluation of Maturation Pathway. Front Immunol. 2020; 11: 1319. https://doi.org/10.3389/fimmu.....
7.
Wolska-Kuśnierz B, Gregorek H, Chrzanowska K, et al. Nijmegen Breakage Syndrome: Clinical and Immunological Features, Long-Term Outcome and Treatment Options – a Retrospective Analysis. J Clin Immunol. 2015; 35(6): 538–549. https://doi.org/10.1007/s10875....
8.
Deripapa E, Balashov D, Rodina Y, et al. Prospective Study of a Cohort of Russian Nijmegen Breakage Syndrome Patients Demonstrating Predictive Value of Low Kappa-Deleting Recombination Excision Circle (KREC) Numbers and Beneficial Effect of Hematopoietic Stem Cell Transplantation (HSCT). Front Immunol. 2017; 8: 807. https://doi.org/10.3389/fimmu.....
9.
Aleinikova O, Fedorova A, Sharapova S. Should Allogeneic Hematopoietic Stem Cell Transplantation be a Treatment Option for Patients with Nijmegen Breakage Syndrome? Belarusian Experience. Cell Ther Transplant. 2015; 4(1–2): 31–37. https://doi.org/10.18620/1866-....
10.
Maurer MH, Hoffmann K, Sperling K, Varon R. High prevalence of the NBN gene mutation c.657–661del5 in Southeast Germany. J Appl Genet. 2010; 51(2): 211–214. https://doi.org/10.1007/BF0319....
11.
Kocheva SA, Martinova K, Antevska-Trajkova Z, Coneska-Jovanova B, Eftimov A, Dimovski AJ. T-lymphoblastic leukemia/lymphoma in macedonian patients with Nijmegen breakage syndrome. Balkan J Med Genet. 2016; 19(1): 91–94. https://doi.org/10.1515/bjmg-2....
12.
von der Hagen M, Pivarcsi M, Liebe J, et al. Diagnostic approach to microcephaly in childhood: a two-center study and review of the literature. Dev Med Child Neurol. 2014; 56(8): 732–741. https://doi.org/10.1111/dmcn.1....
13.
Borte S, von Döbeln U, Fasth A, et al. Neonatal screening for severe primary immunodeficiency diseases using high-throughput triplex real-time PCR. Blood. 2012; 119(11): 2552–2555. https://doi.org/10.1182/blood-....
14.
van der Burg M, Mahlaoui N, Gaspar HB, Pai SY. Universal Newborn Screening for Severe Combined Immunodeficiency (SCID). Front Pediatr. 2019; 7: 373. https://doi.org/10.3389/fped.2....
15.
Giżewska M, Durda K, Winter T, et al. Newborn Screening for SCID and Other Severe Primary Immunodeficiency in the Polish-German Transborder Area: Experience From the First 14 Months of Collaboration. Front Immunol. 2020; 11: 1948. https://doi.org/10.3389/fimmu.....
16.
Patel JP, Puck JM, Srinivasan R, et al. Nijmegen breakage syndrome detected by newborn screening for T cell receptor excision circles (TRECs). J Clin Immunol. 2015; 35(2): 227–233. https://doi.org/10.1007/s10875....
17.
Puck JM. Newborn screening for severe combined immunodeficiency and T-cell lymphopenia. Immunol Rev. 2019; 287(1): 241–252. https://doi.org/10.1111/imr.12....
18.
Patel JP, Puck JM, Srinivasan R, et al. Nijmegen breakage syndrome detected by newborn screening for T cell receptor excision circles (TRECs). J Clin Immunol. 2015; 35(2): 227–33.
19.
Attarbaschi A, Carraro E, Ronceray L, et al. Second malignant neoplasms after treatment of non-Hodgkin’s lymphoma-a retrospective multinational study of 189 children and adolescents. Leukemia. 2021; 35(2): 534–549. https://doi.org/10.1038/s41375....
20.
Buchbinder D, Hauck F, Albert MH, et al. Rubella Virus-Associated Cutaneous Granulomatous Disease: a Unique Complication in Immune-Deficient Patients, Not Limited to DNA Repair Disorders. J Clin Immunol. 2019; 39(1): 81–89. https://doi.org/10.1007/s10875....
21.
Bonilla FA. Update: Vaccines in primary immunodeficiency. J Allergy Clin Immunol. 2018; 141(2): 474–481. https://doi.org/10.1016/j.jaci....
22.
Mosor M, Ziółkowska-Suchanek I, Nowicka K, Dzikiewicz-Krawczyk A, Januszkiewicz-Lewandowska D, Nowak J. Germline variants in MRE11/RAD50/NBN complex genes in childhood leukemia. BMC Cancer. 2013; 13: 457. https://doi.org/10.1186/1471-2....
23.
Gao P, Ma N, Li M, Tian QB, Liu DW. Functional variants in NBS1 and cancer risk: evidence from a meta-analysis of 60 publications with 111 individual studies. Mutagenesis. 2013; 28(6): 683–697. https://doi.org/10.1093/mutage....
24.
di Masi A, Berardinelli F, Lli DE, Antoccia A. Cancer proneness in Nijmegen Breakage Syndrome Carriers. In: Neri Ch, editor. Advances in Genome Science. Probing Intracellular Regulation; 2013. p. 101–119.
25.
Dzikiewicz-Krawczyk A, Mosor M, Januszkiewicz D, Nowak J. Impact of heterozygous c.657–661del, p.I171V and p.R215W mutations in NBN on nibrin functions. Mutagenesis. 2012; 27(3): 337–343. https://doi.org/10.1093/mutage....
26.
Habib R, Kim R, Neitzel H, et al. Telomere attrition and dysfunction: a potential trigger of the progeroid phenotype in nijmegen breakage syndrome. Aging (Albany NY). 2020; 12(12): 12342–12375. https://doi.org/10.18632/aging....
27.
Gregorek H, Chrzanowska KH, Dzierzanowska-Fangrat K, et al. Nijmegen breakage syndrome: Long-term monitoring of viral and immunological biomarkers in peripheral blood before development of malignancy. Clin Immunol. 2010; 135(3): 440–447. https://doi.org/10.1016/j.clim....
28.
Maciejczyk M, Mikoluc B, Pietrucha B, et al. Oxidative stress, mitochondrial abnormalities and antioxidant defense in Ataxia-telangiectasia, Bloom syndrome and Nijmegen breakage syndrome. Redox Biol. 2017; 11: 375–383. https://doi.org/10.1016/j.redo....
29.
Maciejczyk M, Heropolitanska-Pliszka E, Pietrucha B, et al. Antioxidant Defense, Redox Homeostasis, and Oxidative Damage in Children With Ataxia Telangiectasia and Nijmegen Breakage Syndrome. Front Immunol. 2019; 10: 2322. https://doi.org/10.3389/fimmu.....
30.
Pietrucha B, Heropolitanska-Pliszka E, Maciejczyk M, et al. Comparison of Selected Parameters of Redox Homeostasis in Patients with Ataxia-Telangiectasia and Nijmegen Breakage Syndrome. Oxid Med Cell Longev. 2017; 2017: 6745840. https://doi.org/10.1155/2017/6....
31.
Salewsky B, Hildebrand G, Rothe S, et al. Directed Alternative Splicing in Nijmegen Breakage Syndrome: Proof of Principle Concerning ItsTherapeutical Application. Mol Ther. 2016; 24(1): 117–124. https://doi.org/10.1038/mt.201....
32.
Attarbaschi A, Carraro E, Abla O, et al. Non-Hodgkin lymphoma and pre-existing conditions: spectrum, clinical characteristics and outcome in 213 children and adolescents. Haematologica. 2016; 101(12): 1581–1591. https://doi.org/10.3324/haemat....
33.
Mellgren K, Attarbaschi A, Abla O, et al. Non-anaplastic peripheral T cell lymphoma in children and adolescents-an international review of 143 cases. Ann Hematol. 2016; 95(8): 1295–1305. https://doi.org/10.1007/s00277....
34.
Schütte P, Möricke A, Zimmermann M, et al. Preexisting conditions in pediatric ALL patients: Spectrum, frequency and clinical impact. Eur J Med Genet. 2016; 59(3): 143–151. https://doi.org/10.1016/j.ejmg....
35.
Dembowska-Baginska B, Perek D, Brozyna A, et al. Non-Hodgkin lymphoma (NHL) in children with Nijmegen Breakage syndrome (NBS). Pediatr Blood Cancer. 2009; 52(2): 186–190. https://doi.org/10.1002/pbc.21....
36.
Fedorova A, Sharapova S, Mikhalevskaya T, et al. Non-Hodgkin Lymphoma in Children with Primary Immunodeficiencies: Clinical Manifestations, Diagnosis, and Management, Belarusian Experience. Lymphoma. 2015; 2015: 1–10. https://doi.org/10.1155/2015/1....
37.
Pastorczak A, Szczepanski T, Mlynarski W; International Berlin-Frankfurt-Munster (I-BFM) ALL host genetic variation working group. Clinical course and therapeutic implications for lymphoid malignancies in Nijmegen breakage syndrome. Eur J Med Genet. 2016; 59(3): 126–132. https://doi.org/10.1016/j.ejmg....
38.
Lehrnbecher T, Averbuch D, Castagnola E, et al. 8th European Conference on Infections in Leukaemia: 2020 guidelines for the use of antibiotics in paediatric patients with cancer or post-haematopoietic cell transplantation. Lancet Oncol. 2021; 22(6): e270-e280. https://doi.org/10.1016/S1470-....
39.
Groll AH, Pana D, Lanternier F, et al. 8th European Conference on Infections in Leukaemia: 2020 guidelines for the diagnosis, prevention, and treatment of invasive fungal diseases in paediatric patients with cancer or post-haematopoietic cell transplantation. Lancet Oncol. 2021; 22(6): e254-e269. https://doi.org/10.1016/S1470-....
40.
Bienemann K, Burkhardt B, Modlich S, et al. Promising therapy results for lymphoid malignancies in children with chromosomal breakage syndromes (Ataxia teleangiectasia or Nijmegen-breakage syndrome): a retrospective survey. Br J Haematol. 2011; 155(4): 468–476. https://doi.org/10.1111/j.1365....
41.
Zawitkowska J, Lejman M, Zaucha-Prażmo A, et al. Grade 3 and 4 Toxicity Profiles During Therapy of Childhood Acute Lymphoblastic Leukemia. In Vivo. 2019; 33(4): 1333–1339. https://doi.org/10.21873/inviv....
42.
Landmann E, Burkhardt B, Zimmermann M, et al. Results and conclusions of the European Intergroup EURO-LB02 trial in children and adolescents with lymphoblastic lymphoma. Haematologica. 2017; 102(12): 2086–2096. https://doi.org/10.3324/haemat....
43.
Kara B, Koksal Y. Pediatric Lymphoma and Solid Tumors Associated With Cancer Susceptibility Syndromes. J Pediatr Hematol Oncol. 2020; 42(7): 438–445. https://doi.org/10.1097/MPH.00....
44.
Włodarczyk M, Lejman M. Chromosomal instability associated with adverse outcome: a case report of patient with Nijmegen breakage syndrome and rapidly developed T-NHL with complex karyotype. Mol Cytogenet. 2020 Aug 20; 13: 35. https://doi.org/10.1186/s13039.... PMID: 32843899; PMCID: PMC7441545.
45.
Tomasik B, Pastorczak A, Fendler W, et al. Heterozygous carriers of germline c.657_661del5 founder mutation in NBN gene are at risk of central nervous system relapse of B-cell precursor acute lymphoblastic leukemia. Haematologica. 2018; 103(5): e200-e203. https://doi.org/10.3324/haemat....
46.
Baleydier F, Bernard F, Ansari M. The Possibilities of Immunotherapy for Children with Primary Immunodeficiencies Associated with Cancers. Biomolecules. 2020; 10(8): 1112. https://doi.org/10.3390/biom10....
47.
Kyriakidis I, Vasileiou E, Rossig C, Roilides E, Groll AH, Tragiannidis A. Invasive Fungal Diseases in Children with Hematological Malignancies Treated with Therapies That Target Cell Surface Antigens: Monoclonal Antibodies, Immune Checkpoint Inhibitors and CAR T-Cell Therapies. J Fungi (Basel). 2021; 7(3): 186. https://doi:10.3390/jof7030186.
48.
Verhoeven D, Stoppelenburg AJ, Meyer-Wentrup F, Boes M. Increased risk of hematologic malignancies in primary immunodeficiency disorders: opportunities for immunotherapy. Clin Immunol. 2018; 190: 22–31. https://doi:10.1016/j.clim.201....
49.
Rubinstein JD, Burns K, Absalon M, et al. EBV-directed viral-specific T-lymphocyte therapy for the treatment of EBV-driven lymphoma in two patients with primary immunodeficiency and DNA repair defects. Pediatr Blood Cancer. 2020; 67(3): e28126. https://doi.org/10.1002/pbc.28....
50.
June CH, O’Connor RS, Kawalekar OU, Ghassemi S, Milone MC. CAR T cell immunotherapy for human cancer. Science. 2018; 359(6382): 1361–1365. https://doi:10.1126/science.aa....
51.
Queudeville M, Ebinger M. Blinatumomab in Pediatric Acute Lymphoblastic Leukemia-From Salvage to First Line Therapy (A Systematic Review). J Clin Med. 2021; 10(12): 2544. https://doi:10.3390/jcm1012254....
52.
Frey N. Cytokine release syndrome: Who is at risk and how to treat. Best Pract Res Clin Haematol. 2017; 30(4): 336–340. https://doi:10.1016/j.beha.201....
53.
Schlegel P, Lang P, Zugmaier G, et al. Pediatric posttransplant relapsed/refractory B-precursor acute lymphoblastic leukemia shows durable remission by therapy with the T-cell engaging bispecific antibody blinatumomab. Haematologica. 2014; 99(7): 1212–1219. https://doi:10.3324/haematol.2....
54.
Slack J, Albert MH, Balashov D, et al. Outcome of hematopoietic cell transplantation for DNA double-strand break repair disorders. J Allergy Clin Immunol. 2018; 141(1): 322–328.e10. https://doi.org/10.1016/j.jaci....
55.
Woźniak M, Krzywoń M, Hołda MK, Goździk J. Reduced-intensity conditioning umbilical cord blood transplantation in Nijmegen breakage syndrome. Pediatr Transplant. 2015; 19(2): E51-E55. https://doi.org/10.1111/petr.1....
56.
Laberko A, Sultanova E, Gutovskaya E, et al. Treosulfan-Based Conditioning Regimen in Haematopoietic Stem Cell Transplantation with TCRαβ/CD19 Depletion in Nijmegen Breakage Syndrome. J Clin Immunol. 2020; 40(6): 861–871. https://doi.org/10.1007/s10875....
57.
Gałązka P, Czyżewski K, Szaflarska-Popławska A, Dębski R, Krenska A, Styczyński J. Complex profile of multiple hepatobiliary and gastrointestinal complications after hematopoietic stem cell transplantation in a child with Nijmegen breakage syndrome. Cent Eur J Immunol. 2019; 44(3): 327–331. https://doi.org/10.5114/ceji.2....
58.
Moser O, Zimmermann M, Meyer U, et al. Second malignancies after treatment of childhood non-Hodgkin lymphoma: a report of the Berlin-Frankfurt-Muenster study group. Haematologica. 2021; 106(5): 1390–1400. https://doi.org/10.3324/haemat....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.