Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Assessment of hospitalizations of patients after intoxication with organophosphates used in agriculture
1
Toxicology Clinic, Medical University, Lublin, Poland
2
Faculty of Human Sciences, University of Economics and Innovation, Lublin, Poland
3
Clinical Department of Toxicology and Cardiology, Stefan Wyszyński Regional Specialist Hospital, Lublin, Poland
Ann Agric Environ Med. 2022;29(1):143-148
KEYWORDS
TOPICS
- Health effects of chemical pollutants in agricultural areas , including occupational and non-occupational effects of agricultural chemicals (pesticides, fertilizers) and effects of industrial disposal (heavy metals, sulphur, etc.) contaminating the atmosphere, soil and water
- Work-related accidents and injuries in agriculture, forestry, food industry and wood industry: incidence, causes, social aspects and prevention
ABSTRACT
Introduction:
Clinical manifestation of organophosphates toxicity may be differentiate and include cholinergic toxidrome, intermediate syndrome, OP-induced delayed polyneuropathy to chronic OP-induced neuropsychiatric disorder (OPIDN). Patients symptoms, along with decrease in cholinesterase serum level, determines the possible diagnosis of organophosphate poisoning.
Objective:
The aim of the study was to present the clinical manifestation and cholinesterase level changes in intoxication with organophosphorus compounds in patients.
Material and methods:
A data base was created by analysis of the hospital documents of 34 patients hospitalized due to organophosphate intoxication. Statistical analysis involved frequency tables with percentage values, the application of non-parametric Chi-square test and parametric t-Student test (with homogeneity of variance Levine test). The level of static significance was set to p=0.05.
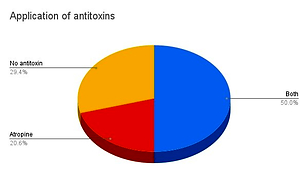
Results:
In fatal hospitalizations (20.6%), cholinesterase level was significantly lower (265.87 U/l) than in other patients (4254.78 U/l; p<0.05). Similarly, levels of cholinesterase were decreased in group of patients with acute respiratory failure (999.79 U/l vs 4943.86 U/l in other patients; p<0.05), patients with multi-organ dysfunction syndrome (244.13 U/l vs 4914.89 U/l in other patients; p<0.05) and those with cardiac arrest (547 U/l vs 4636.25 U/l in other patients). A statistically significant difference was also observed in cholinesterase level of patients who required mechanical ventilation (548.17 U/l vs 5219.71 U/l in other group). The study revealed that 29.4% of poisonings were suicidal
Conclusions:
The management of a patient with organophosphate poisoning remains challenging and requires continuous control. A significant step in the diagnostic process is the assessment changes in both the clinical picture and cholinesterase level.
Clinical manifestation of organophosphates toxicity may be differentiate and include cholinergic toxidrome, intermediate syndrome, OP-induced delayed polyneuropathy to chronic OP-induced neuropsychiatric disorder (OPIDN). Patients symptoms, along with decrease in cholinesterase serum level, determines the possible diagnosis of organophosphate poisoning.
Objective:
The aim of the study was to present the clinical manifestation and cholinesterase level changes in intoxication with organophosphorus compounds in patients.
Material and methods:
A data base was created by analysis of the hospital documents of 34 patients hospitalized due to organophosphate intoxication. Statistical analysis involved frequency tables with percentage values, the application of non-parametric Chi-square test and parametric t-Student test (with homogeneity of variance Levine test). The level of static significance was set to p=0.05.
Results:
In fatal hospitalizations (20.6%), cholinesterase level was significantly lower (265.87 U/l) than in other patients (4254.78 U/l; p<0.05). Similarly, levels of cholinesterase were decreased in group of patients with acute respiratory failure (999.79 U/l vs 4943.86 U/l in other patients; p<0.05), patients with multi-organ dysfunction syndrome (244.13 U/l vs 4914.89 U/l in other patients; p<0.05) and those with cardiac arrest (547 U/l vs 4636.25 U/l in other patients). A statistically significant difference was also observed in cholinesterase level of patients who required mechanical ventilation (548.17 U/l vs 5219.71 U/l in other group). The study revealed that 29.4% of poisonings were suicidal
Conclusions:
The management of a patient with organophosphate poisoning remains challenging and requires continuous control. A significant step in the diagnostic process is the assessment changes in both the clinical picture and cholinesterase level.
REFERENCES (26)
1.
Hoffman RS, Howland MA, Lewin NA, et al. Goldfrank’s Toxicologic Emergencies, Insectidices: organic phosphorous compounds and carbamates, 2019: 1409–1420.
3.
Suratman S, Edwards JW, Babina K. Organophosphate pesticides exposure among farmworkers: pathways and risk of adverse health effects. Rev Environ Health. 2015; 30(1): 65–79. https://doi.org/10.1515/ reveh-2014-0072.
4.
Raveendra K R, Mohan C N, Nandan Kodur. A study to assess the utility of peradeniya organophosphorous poisoning (POP) scale, poisoning severity score (PSS) and glasgow coma scale (GCS) in predicting severity and treatment outcome in acute organophosphorous poisoning. International J Contemp Med Res. 2020; 7(2): B20-B24. https://doi. org/10.21276/ijcmr.2020.7.2.22.
5.
Robb EL, Baker MB. Organophosphate Toxicity. [Updated 2020 Jul 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/b... NBK470430/.
6.
Sprawozdanie z realizacji w latach 2018–2019 krajowego planu działania na rzecz ograniczenia ryzyka związanego ze stosowaniem środków ochrony roślin na lata 2018–2022, https://www.gov.pl/web/rolnict... krajowy-plan-dzialania-na-rzecz-ograniczenia-ryzyka-zwiazanego-ze-stosowaniem-srodkow-ochrony-roslin (accessed: 27.10.2020).
7.
Petreski T, Kit B, Strnad M, Grenc D, Svenšek F. Cholinergic syndrome: a case report of acute organophosphate and carbamate poisoning. Arh Hig Rada Toksikol. 2020; 71(2): 163–166. https://doi.org/10.2478/ aiht-2020-71-3413.
8.
Jokanović M. Neurotoxic effects of organophosphorus pesticides and possible association with neurodegenerative diseases in man: A review. Toxicology. 2018; 410: 125–131. https://doi.org/10.1016/j.tox.....
9.
Lott EL, Jones EB. Cholinergic Toxicity. [Updated 2021 May 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/b... NBK539783/.
10.
Reddy BS, Skaria TG, Polepalli S, et al. Factors associated with outcomes in organophosphate and carbamate poisoning: a retrospective study. Toxicol Res. 2020; 36(3): 257–266. https://doi.org/10.1007/s43188...- 00029-x.
11.
anjay A, Siddheshwar V, Sheshrao S. The Clinico-Demographic Study of Morbidity and Mortality in Patients with Organophosphate Compound Poisoning at Tertiary Care Hospital in Rural India. Int J Adv Med. 2017; 4: 809–818. https://doi.org/10.18203/2349-.... ijam20172277.
12.
Aygun D, Doganay Z, Altintop L, et al. Serum acetylcholinesterase and prognosis of acute organophosphate poisoning. J Toxicol Clin Toxicol. 2002; 40(7): 903–910. https://doi.org/10.1081/clt-12....
13.
King AM, Aaron CK. Organophosphate and carbamate poisoning. Emerg Med Clin North Am. 2015; 33(1): 133–151. https://doi. org/10.1016/j.emc.2014.09.010.
14.
London L, Flisher AJ, Wesseling C, Mergler D, Kromhout H. Suicide and exposure to organophosphate insecticides: cause or effect? Am J Ind Med. 2005; 47(4): 308–321. https://doi.org/10.1002/ajim.2....
15.
Lee YH, Oh YT, Lee WW, et al. The association of alcohol consumption with patient survival after organophosphate poisoning: a multicenter retrospective study. Intern Emerg Med. 2017; 12(4): 519–526. https:// doi.org/10.1007/s11739-016-1484-9.
16.
Karakus A, Celik MM, Karcioglu M, Tuzcu K, Erden ES, Zeren C. Cases of organophosphate poisoning treated with high-dose of atropine in an intensive care unit and the novel treatment approaches. Toxicol Ind Health. 2014; 30(5): 421–425. https://doi.org/10.1177/074823....
17.
Patil G, Murthy N, Nikhil M. Contributing Factors for Morbidity and Mortality in Patients with Organophosphate Poisoning on Mechanical Ventilation: A Retrospective Study in a Teaching Hospital. J Clin Diagn Res. 2016; 10(12): UC18-UC20. https://doi.or /10.7860/ JCDR/2016/22116.9038.
18.
Abou-Donia MB, Siracuse B, Gupta N, Sobel Sokol A. Sarin (GB, O-isopropyl methylphosphonofluoridate) neurotoxicity: critical review. Crit Rev Toxicol. 2016; 46(10): 845–875. https://doi.org/10.1080/1040 8444.2016.1220916.
19.
Peter JV, Sudarsan TI, Moran JL. Clinical features of organophosphate poisoning: A review of different classification systems and approaches. Indian J Crit Care Med. 2014; 18(11): 735–745. https:// doi.org/10.4103/0972-5229.144017.
20.
Cha YS, Kim H, Go J, et al. Features of myocardial injury in severe organophosphate poisoning. Clin Toxicol (Phila). 2014; 52(8): 873–879. https://doi.org/10.3109/155636....
21.
Shiba M, Kato T, Morimoto T, et al. Serum cholinesterase as a prognostic biomarker for acute heart failure. Eur Heart J Acute Cardiovasc Care. 2021; 10(3): 335–342. https://doi.org/10.1093/ehjacc....
22.
Gunasena JB, De Silva ST. Organophosphate Poisoning Complicated by Rhabdomyolysis-Induced Acute Kidney Injury: A Case Report and Review of Literature. J Clin Toxicol. 2020; 10(5): 1000450. https://dx.doi. org/10.35248/2161-0495.20.10.450.
23.
John M, Oommen A, Zachariah A. Muscle injury in organophosphorous poisoning and its role in the development of intermediate syndrome. Neurotoxicology. 2003; 24(1): 43–53. https://doi.org/10.1016/s0161- 813x(02)00111-0.
24.
Kumar GC, Bhuvana K, Venkatarathnamma PN, Sarala N. Serum creatine phosphokinase as predictor of intermediate syndrome in organophosphorus poisoning. Indian J Crit Care Med. 2015; 19(7): 384–387. https://doi.org/10.4103/0972-5....
25.
Balali-Mood M, Saber H. Recent advances in the treatment of organophosphorous poisonings. Iran J Med Sci. 2012; 37(2): 74–91.
26.
Eyer F, Worek F, Eyer P, et al. Obidoxime in acute organophosphate poisoning: 1 – clinical effectiveness. Clin Toxicol (Phila). 2009; 47(8): 798–806. https://doi.org/10.1080/155636....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.