Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Nosocomial infections as one of the most important problems of healthcare system.
1
Project InterDoktorMen, Medical University of Lodz, Poland
2
Laboratory of Epidemiology, Military Institute of Hygiene and Epidemiology (WIHE), Warsaw, Poland
3
Institute of Environmental Engineering, Poznan University of Technology, Poland
4
Department of Management, University of Technology of Lodz, Poland
5
Department of Medical Insurance and Health Care Financing, Medical University of Lodz, Poland
6
Department of Management and Logistics in Health Care, Medical University of Lodz, Poland
Ann Agric Environ Med. 2021;28(3):361-366
KEYWORDS
TOPICS
ABSTRACT
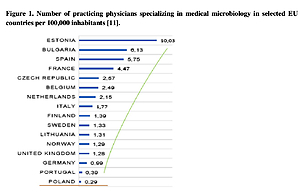
Healthcare-associated infections (HAI) are commonly defined as adverse events resulting from the provision of healthcare. The reduction of risk arising from the spread of pathogenic microorganisms in the hospital environment is a considerable challenge in the context of the proper functioning of the medical services sector. The financial costs of hospitals resulting from HAI are a serious problem for the Polish healthcare system. The spread of strains with a high level of drug resistance in individual hospitals is associated with the local epidemiological situation. In 2015–2017, there was a high increase in the number of infections caused by New Delhi strains. The highest increase due to this strain occurred in Mazowieckie and Podlasie provinces. The dynamics of infection caused by New Delhi strains throughout Poland in 2015–2016 indicated
an increase of 278.7%. In 2017, the phenomenon of antibiotic abuse in all regions of Poland was 24% higher than the EU average. One of the reasons is the insufficient number of diagnostic tests ordered by both general practitioners and doctors representing hospital care. In 2016–2017, the average number of microbiological tests in diagnosing hospital infections performed annually within the entire territory of Poland was 50% lower than in European Union countries and the number recommended by WHO. Increased, and at the same time inappropriate antibiotic therapy led to a build-upof drug resistance among bacterial species of significant clinical importance. The current epidemiological situation imposes the necessity for constant HAI control and broadly understood rationalization of the guidelines of hospital antibiotic policy.
REFERENCES (54)
1.
Larypoor M, Frsad S. Evaluation of nosocomial infections in one of hospitals of Qom, 2008. Iran J Med Microbiol. Persian. 2011; 5(3): 7–17.
2.
Olise CC, Simon-Oke IA, et al. Fomites: Possible vehicle of nosocomial infections. J Pub Health Catalog. 2018; 1(1): 16–16.
3.
Dobrosielska-Matusik KM, Pilecki W. Problem szpitalnych zakażeń krwi u pacjentów hospitalizowanych na oddziałach intensywnej terapii. Piel Zdr Publ. 2019; 9(1): 63–70.
4.
Kiersnowska Z, Lemiech-Mirowska E, Ginter-Kramarczyk D, Kruszelnicka I, Michałkiewicz M, Marczak M. Problems of Clostridium difficile infection (CDI) in Polish healthcare units. Ann Agric Environ Med. 2020. doi:10.26444/aaem/119321.
5.
Bulanda M, Burzyńska B, Ciążyński M, Deptuła A, Dębicka B, Dubiel G, at. al. System kontroli zakażeń związanych z opieką zdrowotną w Polsce. Stowarzyszenie Epidemiologii Szpitalnej. 2016.
6.
Dudzik-Urbaniak E, Kutaj-Wąsikowska H, Kutryba B, Piotrowski M. Program Akredytacji – Szpitale, zestaw standardów; 2016.
7.
Dz.U. 2019, poz. 1239. Obwieszczenie Marszałka Sejmu Rzeczypospolitej Polskiej z dnia 6 czerwca 2019 r. w sprawie ogłoszenia jednolitego tekstu ustawy o zapobieganiu oraz zwalczaniu zakażeń i chorób zakaźnych u ludzi.
8.
PN EN 15244:2013. Usługi sektora ochrony zdrowia – Systemy zarządzania jakością – Wymagania oparte na EN ISO 9001:2015.
10.
Osińska M, Rysiak E, Zaręba R, Worona P, Kazberuk A, Prokop I, Celińska-Janowicz K, Zaręba I. Zakażenia szpitalne w aspekcie prawnym. Anestezjologia i Ratownictwo 2018; 12: 353–356.
11.
Dziewa AM, Ksykiewicz-Dorota A. Methods of monitoring and registration of hospital infections. Hygeia Public Health 2012; 47(1): 56–63.
12.
Sadowska M. Cause-and effectrelationship as the premise of provider’sliability for hospital-acquiredinfection. Studia Prawnicze KUL. 2017:3,71,107–120.
15.
ECDC. Europa. EU. Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals 2011–2012.
16.
Janowicz R. Ograniczenie zakażeń szpitalnych z wykorzystaniem środków architektonicznych. Wydawnictwo Wydziału Architektury Politechniki Gdańskiej, pp. 209. ISBN. 2019; 978–83–64333–27–9.
17.
Najwyższa Izba Kontroli. Zakażenia w podmiotach leczniczych. Lata 2016–2017 (I półrocze).
18.
Elliott C. Justiz-Vaillant A. Nosocomial Infections: A 360-degree Review. Int Biol Biomed J. 2018; 4(2): 72–81.
19.
Stanek J, Zyzik R. Prevention of healthcare associated infections – behavioural perspective. Hygeia Public Health. 2018;53 (4): 333–339.
20.
Umar D, Basheer B, Husain A, et al. Evaluation of bacterial contamination in a clinical environment. J Int Oral Health 2015; 7(1): 53–5.
23.
Haque M, Sartelli M, McKimm J, Bakar MA. Health care-associated infections – an overview. Infect Drug Resistance. 2018; 11: 2321–2333.
24.
Farahani A, Mohajeri P, Soltani S, Getso MI, Khatib M, Dastranj M. Investigation of bio-air contamination in some hospitals of Kermanshah, Iran. Adv Human Biol. 2019;9(1):65. doi:10.4103/aihb.aihb_49_18.
25.
Sadowska M. Cause-and effectrelationship as the premise of provider’sliability for hospital-acquiredinfection). Studia Prawnicze KUL, 2017; 3(71): 107–120.
26.
Wilson AP, Livermore DM, Otter JA, et al. Prevention and control of multi-drug- -resistant Gram-negative bacteria: recommendations from a Joint Working Party. J Hosp Infect. 2016; 92(Suppl. 1): S1– S44.
27.
World Health Organization. Health care-associated infections. Fact sheet. WHO. www.who.int/gpsc/country_work/….
28.
Tolera M, Degu A, Dheresa M, Marami D. Bacterial Nosocomial Infections and Antimicrobial Susceptibility Pattern among Patients Admitted at Hiwot Fana Specialized University Hospital, Eastern Ethiopia. Hindawi Adv Med. 2018, Article ID 2127814,7. DOI:0.1155/2018/2127814.
29.
Suetens C, Latour K, Kärki T, Ricchizzi E, Kinross P, Moro ML, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. 2018; 23(46): pii=1800516. DOI:10.2807/1560–7917.ES.2018.23.46.1800516.
30.
Craig A, et al. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs, Infect Control Hosp Epidemiol. 2011; 32: 101–14.
31.
Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: A meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013; 173: 2039–46.
32.
Baraniak A, Izdepski R, Fiett J, Gawryszewska I, Bojarska K, Herda M, Literacka E. NDM-producing Enterobacteriaceae in Poland, 2012–14: inter-regional outbreak of Klebsiella pneumoniae ST11 and sporadic cases, J Animicrob Chmother. 2016; 71: 85–91.
33.
Czekaj T, Ciszewski M. Klebsiella pneumoniae NDM – nowa superbakteria. Med Rodz. 2015; 1: 23–27.
34.
Wojkowska-Mach J, Godman B, Glassman, et al. Antibiotic consumption and antimicrobial resistance in Poland; findings and implications, Antimicrob Resist Infect Control. 2018; 7: 136.
35.
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. 2013: 11–21.
36.
Leclercq R. Safeguarding future antimicrobal options: strategies to minimize resistance Clin Microbiol Infect. 2001; 7(3): 18–23.
37.
Markiewicz Z, Kwiatkowski Z. Bakterie, antybiotyki, lekooporność Wyd. Naukowe PWN Warszawa 2006.
38.
Sadkowska-Todys M, Zieliński A, Czarkowski MP. Infectious diseases in Poland in 2017. Prz Epidemiol. 2019; 73(2):135–15.
39.
BAJ J, Markiewicz Z. Biologia molekularna bakterii Wyd. Naukowe PWN Warszawa 2006.
40.
Cooper RM, Tsimring L, Hasty J. Inter-species population dynamics enhance microbial horizontal gene transfer and spread of antibiotic resistance. eLife. 2017; 6: e25950. Published online 2017 Nov 1. doi: 10.7554/eLife.25950.
41.
Kiersnowska Z, Lemiech-Mirowska E, et al. Sytuacja epidemiologiczna w jednostkach ochrony zdrowia, Badania i rozwój Młodych Naukowców w Polsce 2019; 2:13–19.
43.
Nazir A, Kadri SM. An overview of hospital acquired infections and the role of the microbiology laboratory. Int J Res Med Sci. 2014; 2(1): 21– 27.
44.
Chwedoruk M, Gotlib J. Assessment of knowledge of nurses in surgical departments on hospital infections spread by the contact route. Med Og Nauk Zdr. 2014; 20(2): 192–198.
45.
Szymańska-Pomorska G, Pytel A, Smolińska B. Hospitalinfections as a modern hospitalepidemiological problem. Decontamination and rules of medical equipment storage. Piel Zdr Publ. 2017;7(2): 149–152. DOI:10.17219/pzp/75215.
46.
Yu Lü, Min Hong Cai, Jian Cheng J, et al. A multi-center nested case-control study on hospitalization costs and length of stay due to healthcare-associated infection. Antimicrob Resist Infect Control. 2018; 7: 99.
47.
Khan ID, Basu A, Kiran S, Trivedi S, Pandit P, Anupam Ch. Device-Associated Healthcare-Associated Infections (DA-HAI) and the caveat of multiresistance in a multidisciplinary intensive care unit. Med J Armed Forces India. 2017; 73(3): 222–231.
48.
Kołpa M, Wałaszek M, Różańska A, Wolak Z, Wójkowska-Mach J. Hospital-Wide Surveillance of Healthcare-Associated Infections as a Source of Information about Specific Hospital Needs. A 5-Year Observation in a Multiprofile Provincial Hospital in the South of Poland. Int J Environ Res Public Health. 2018 Sep; 15(9): 1956.
49.
Maciejewski D, Misiewska-Kaczur A. Zakażenia w oddziałach intensywnej terapii. In: Zakażenia szpitalne. Ed. D. Dzierżanowska. Media Press, Bielsko-Biała 2008: 249–265.
50.
Sprawozdanie z realizacji Narodowego Programu Ochrony Antybiotyków 2012. www.antybiotyki.edu.pl.
51.
Sołtys-Bolibrzuch K. Prevention of nosocomial infections. sisyphean work of an epidemiological nurse. Zakażenia XXI wieku 2019;2(1):33–39. DOI: 10.31350/zakazenia/2019/1/Z2019002.
52.
Zarb P, Coignard B, Griskeviciene J, et al. The European Centre for Disease Prevention and Control (ECDC) pilot point prevalence survey of healthcare-associated infections and antimicrobial use. Euro Surveill. 2012;17.
53.
Pittet D, et al. Considerations for a WHO European strategy on health-care-associated infection, surveillance, and control. Lancet Infect Dis. 2005;5:242–5.
54.
Duke MT, Kinney S, Daley AJ, Soenarto Y. Reducing hospital-acquired infections and improving the rational use of antibiotics in a developing country: an effectiveness study. Arch Dis Child. 2015; 100(5): 454–459.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.