Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Colonization with drug-resistant pathogens among patients in long-term care facilities and under home hospice care – a cross-sectional study
1
Department of Social Medicine and Public Health, Medical University, Warsaw, Poland
2
Doctoral School, Medical University, Warsaw, Poland
3
Department of Medical Microbiology, Medical University, Warsaw, Poland
Corresponding author
Monika Zasztowt-Sternicka
Department of Social Medicine and Public Health, Medical University of Warsaw, Poland
Department of Social Medicine and Public Health, Medical University of Warsaw, Poland
Ann Agric Environ Med. 2023;30(4):606-610
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The spread of drug-resistant bacteria is deemed a worldwide threat. Patients in long-term care, including those under palliative care, are exposed to a high risk of colonization and infection with drug-resistant pathogens. This refers primarily to long-term care facilities as opposed to home care. A cross-sectional study was carried out between 1 January 2018 – 30 June 2019. The study was approved by the Bioethics Committee at the Medical University of Warsaw (KB/222/2017).
Objective:
The aim of the study was to assess the frequency and type of colonization with drug-resistant pathogens among patients in long-term care facilities and those under home hospice care. An additional aim was evaluation the risk of pathogen transmission according to the type of provided long-term care.
Material and methods:
The study included 129 participants: 68 patients under the care of 3 long-term care facilities in Warsaw, Poland, 42 patients under home hospice care, and 19 household members of hospice patients. All included participants provided written informed consent. Oropharyngeal and rectal swabs were obtained from all participants for microbiological assessment.
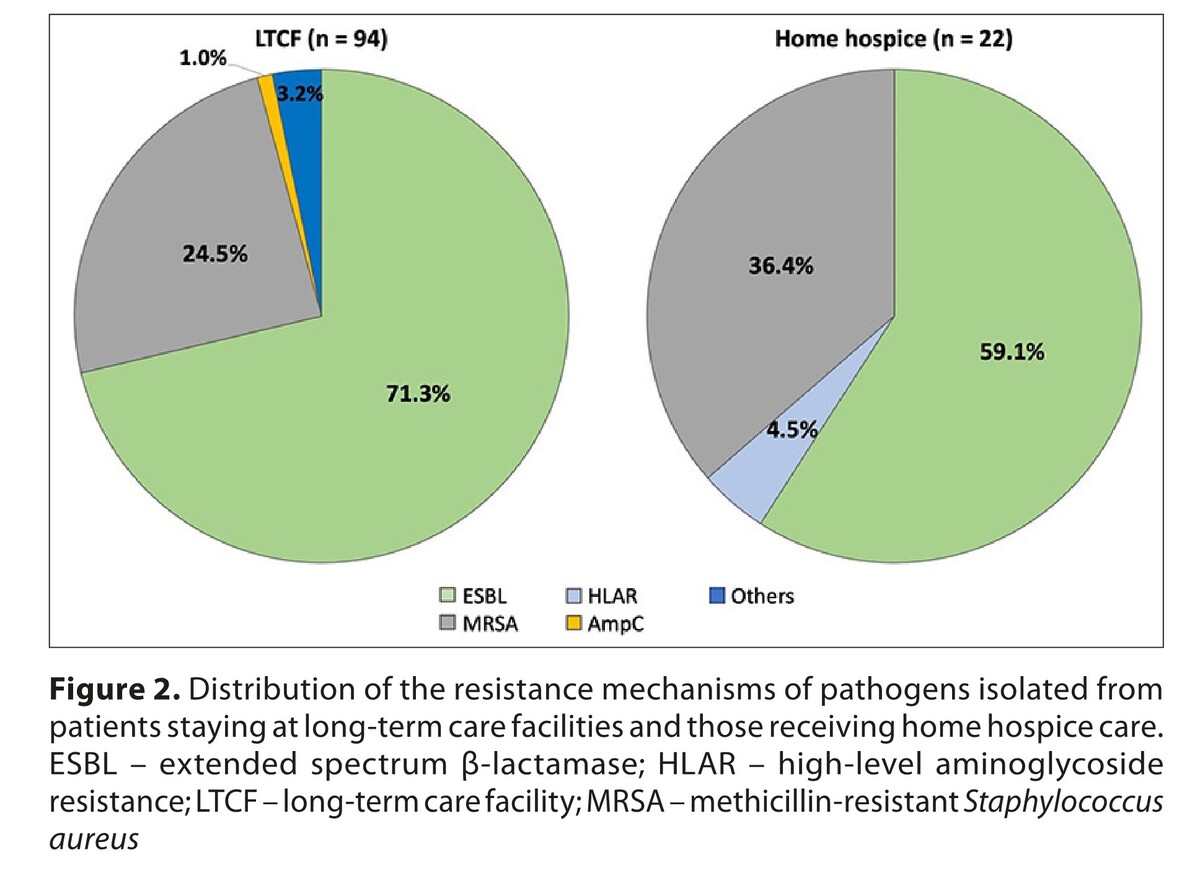
Results:
Colonization with pathogens was more common in long-term care facilities residents (82.4%) than in at-home hospice patients (42.9%). Risk of colonization was significantly lower in patients staying at home than in long-term care facilities patients (OR 0.16; 95% CI 0.06–0.38).
Conclusions:
Conclusions. Risk of colonization with drug-resistant pathogens depends on the type of care and is significantly higher in patients staying at long-term care facilities. Systemic measures, such as microbiological screening, are necessary to provide optimal patient care and to ensure epidemiological safety, both to patients and their caregivers.
The spread of drug-resistant bacteria is deemed a worldwide threat. Patients in long-term care, including those under palliative care, are exposed to a high risk of colonization and infection with drug-resistant pathogens. This refers primarily to long-term care facilities as opposed to home care. A cross-sectional study was carried out between 1 January 2018 – 30 June 2019. The study was approved by the Bioethics Committee at the Medical University of Warsaw (KB/222/2017).
Objective:
The aim of the study was to assess the frequency and type of colonization with drug-resistant pathogens among patients in long-term care facilities and those under home hospice care. An additional aim was evaluation the risk of pathogen transmission according to the type of provided long-term care.
Material and methods:
The study included 129 participants: 68 patients under the care of 3 long-term care facilities in Warsaw, Poland, 42 patients under home hospice care, and 19 household members of hospice patients. All included participants provided written informed consent. Oropharyngeal and rectal swabs were obtained from all participants for microbiological assessment.
Results:
Colonization with pathogens was more common in long-term care facilities residents (82.4%) than in at-home hospice patients (42.9%). Risk of colonization was significantly lower in patients staying at home than in long-term care facilities patients (OR 0.16; 95% CI 0.06–0.38).
Conclusions:
Conclusions. Risk of colonization with drug-resistant pathogens depends on the type of care and is significantly higher in patients staying at long-term care facilities. Systemic measures, such as microbiological screening, are necessary to provide optimal patient care and to ensure epidemiological safety, both to patients and their caregivers.
FUNDING
Funding and conflicts of interest. The research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The Authors declare that there are no conflicts of interest.
Data sharing. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments Language and editorial assistance was provided by Proper Medical Writing, Warsaw, Poland.
REFERENCES (27)
1.
Bloom DE, Chatterji S, Kowal P, et al. Macroeconomic implications of population ageing and selected policy responses. Lancet. 2015;385:649–657.
2.
Augustyn M, Błędowski P, Wyrwicka K, et al. Working Group for the Preparation of the Act on Insurance against the Risk of Independence [in Polish]. http://rszarf.ips.uw.edu.pl/ki... (2010, accessed: 10 July 2021).
3.
Narodowy Fundusz Zdrowia. Nursing and care benefits – long-term care [in Polish]. https://www.nfz-szczecin.pl/ge... (updated 2020, accessed: 21 July 2021).
4.
World Health Organization. Antibiotic resistance. https://www.who.int/news-room/... (2020, accessed: 23 May 2020).
5.
Aslam B, Wang W, Arshad MI, et al. Antibiotic resistance: a rundown of a global crisis. Infect Drug Resist. 2018;11:1645–1658.
6.
Giedraitiene A, Vitkauskiene A, Naginiene R, Pavilonis A. Antibiotic resistance mechanisms of clinically important bacteria. Medicina (Kaunas). 2011;47:137–146.
7.
Surveillance report. Surveillance of antimicrobial resistance in Europe 2017. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). https://www.ecdc.europa.eu/sit... (2017, accessed: 26 May 2020).
8.
Freitas AR, Novais C, Duarte B, et al. High rates of colonisation by ampicillin-resistant enterococci in residents of long-term care facilities in Porto, Portugal. Int J Antimicrob Agents. 2018;51:503–507.
9.
Giufre M, Ricchizzi E, Accogli M, et al. Colonization by multidrug-resistant organisms in long-term care facilities in Italy: a point-prevalence study. Clin Microbiol Infect. 2017;23:961–967.
10.
Heudorf U, Boehlcke K, Schade M. Healthcare-associated infections in long-term care facilities (HALT) in Frankfurt am Main, Germany, January to March 2011. Euro Surveill. 2012;17:20256.
11.
Moro ML, Ricchizzi E, Morsillo F, et al. Infections and antimicrobial resistance in long term care facilities: a national prevalence study. Ann Ig. 2013;25:109–118.
12.
Smith M, Atkins S, Worth L, et al. Infections and antimicrobial use in Australian residential aged care facilities: a comparison between local and international prevalence and practices. Aust Health Rev. 2013;37:529–534.
13.
Stuart RL, Marshall C, Orr E, et al. Members of RACRIG (Residential Aged Care Research Interest Group). Survey of infection control and antimicrobial stewardship practices in Australian residential aged-care facilities. Intern Med J. 2015;45:576–580.
14.
Stuart RL, Wilson J, Bellaard-Smith E, et al. Antibiotic use and misuse in residential aged care facilities. Intern Med J. 2012;42:1145–1149.
15.
Infor. Announcement of the Minister of Health of January 22, 2021 on the publication of a uniform text of the regulation of the Minister of Health on the list of alarm pathogens, registers of hospital infections and alarm pathogens and reports on the current epidemiological situation of the hospital [in Polish]. https://www.infor.pl/akt-prawn... (2021, accessed: 12 July 2021).
16.
Christensen GJ, Bruggemann H. Bacterial skin commensals and their role as host guardians. Benef Microbes. 2014;5:201–215.
17.
Eveillard M, Lafargue S, Guet L, et al. Association between institutionalization and carriage of multiresistant bacteria in the elderly at the time of admission to a general hospital. Eur J Clin Microbiol Infect Dis. 1999;18:133–136.
18.
Verrall A, Merchant R, Dillon J, et al. Impact of nursing home residence on hospital epidemiology of meticillin-resistant Staphylococcus aureus: a perspective from Asia. J Hosp Infect. 2013;83:250–252.
19.
Pulcini C, Clerc-Urmes I, Attinsounon CA, et al. Antibiotic resistance of Enterobacteriaceae causing urinary tract infections in elderly patients living in the community and in the nursing home: a retrospective observational study. J Antimicrob Chemother. 2019;74:775–781.
20.
Gleeson A, Larkin P, Walsh C, O’Sullivan N. Methicillin-resistant Staphylococcus aureus: Prevalence, incidence, risk factors, and effects on survival of patients in a specialist palliative care unit: A prospective observational study. Palliat Med. 2016;30:374–381.
21.
Heckel M, Geissdorfer W, Herbst FA, et al. Nasal carriage of methicillin-resistant Staphylococcus aureus (MRSA) at a palliative care unit: a prospective single service analysis. PLoS One 2017;12:e0188940.
22.
Schmalz O, Strapatsas T, Alefelder C, Grebe SO. Methicillin-resistant Staphylococcus aureus in palliative care: A prospective study of Methicillin-resistant Staphylococcus aureus prevalence in a hospital-based palliative care unit. Palliat Med. 2016;30:703–706.
23.
Ford CD, Lopansri BK, Gazdik MA, et al. The clinical impact of vancomycin-resistant Enterococcus colonization and bloodstream infection in patients undergoing autologous transplantation. Transpl Infect Dis. 2015;17:688–694.
24.
Ford CD, Lopansri BK, Haydoura S, et al. Frequency, risk factors, and outcomes of vancomycin-resistant Enterococcus colonization and infection in patients with newly diagnosed acute leukemia: different patterns in patients with acute myelogenous and acute lymphoblastic leukemia. Infect Control Hosp Epidemiol. 2015;36:47–53.
25.
Kenneley I. Infection control in home healthcare: an exploratory study of issues for patients and providers. Home Healthc Nurse. 2012;30:235–245.
26.
McGoldrick M. Preventing infections in patients using respiratory therapy equipment in the home. Home Healthc Nurse. 2010;28:212–220.
27.
Beltran-Aroca CM, Ruiz-Montero R, Llergo-Munoz A, et al. Impact of the COVID-19 Pandemic on Palliative Care in Cancer Patients in Spain. Int J Environ Res Public Health. 2021;18:11992.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.