Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
Citrobacter freundii and Acinetobacter baumanii infection in a patient with neoplastic lung disease – Case report
1
Department of Epidemiology and Clinical Research Methodology, Medical University, Lublin, Poland
2
Chair and Department of Medical Microbiology, Medical University, Lublin, Poland
3
Student Scientific Association at Department of Epidemiology and Clinical Research Methodology, Medical University, Lublin, Poland
Corresponding author
Karol Lorenc
Student Scientific Association at Department of Epidemiology and Clinical Research Methodology, Medical University, Radziwiłłowska 11, 20-080 Lublin, Poland
Student Scientific Association at Department of Epidemiology and Clinical Research Methodology, Medical University, Radziwiłłowska 11, 20-080 Lublin, Poland
Ann Agric Environ Med. 2021;28(4):724-728
KEYWORDS
TOPICS
ABSTRACT
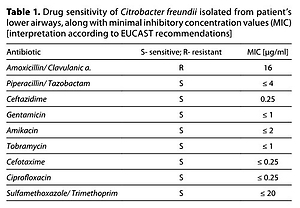
An 85-year-old male with a tumour in his right lung was admitted to Internal Diseases Ward to continue treatment after suffering a sudden cardiac arrest. An empiric antibiotic therapy with amoxycillin was introduced due to increased inflammation markers. Blood and sputum were collected. An abundant growth of AmpC β-lactamase-producing Citrobacter freundii was observed in culture grown from the sputum. The antibiogram showed retained sensitivity to fluoroquinolones. The therapy was modified by replacing β-lactam with ciprofloxacin. Neither clinical nor laboratory improvement were observed. Blood culture indicated sepsis of Acinetobacter baumannii etiology. The strain was suspected of producing OXA carbapenemase (CARBA test positive), KPC (-), MBL (-). Antibiogram illustrated retained sensitivity to gentamicin and colistin with complete resistance to ciprofloxacin. Another modification in treatment was implemented and ciprofloxacin was replaced with colistin.
Citrobacter freundii and Acinetobacter baumanii infection in a patient with neoplastic lung disease – Case report. Doi: 10.26444/aaem/140111
REFERENCES (25)
1.
Didkowska J, Wojciechowska U, Czaderny K, et al. Nowotwory złośliwe w Polsce w 2017 roku. Krajowy Rejestr Nowotworów http://onkologia.org.pl/wp-con... (access: 2020.10.11).
2.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020; 70(1): 7–30. ht tps://doi.org /10.3322/caac.21590.
3.
Rancic M, Ristic L, Stankovic I. Infective complications in patients with lung cancer. Med Pregl. 2010; 63: 643–647. https://doi.org/10.2298/MPNS10....
4.
Ferri M, Ranucci E, Romagnoli P, Giaccone V. Antimicrobial resistance: A global emerging threat to public health systems. Crit Rev Food Sci Nutr. 2017; 57(13): 2857–2876.https://doi.org/10.1080/104083....
5.
Nichols L, Saunders R, Knollmann FD. Causes of death of patients with lung cancer. Arch Pathol Lab Med. 2012; 136(12): 1552–1557.ht t ps://doi.org/10.5858/arpa.2011-0521-OA.
6.
Hayat MJ, Howlader N, Reichman ME, et al. Cancer statistics, trends, and multiple primary cancer analyses from the Surveillance, Epidemiology, and End Results (SEER) Program. Oncologist. 2007; 12 (1): 2 0 –37.https://doi.org/10.1634/theonc....
7.
Mayo Clinic. Diseases and conditions: Lung cancer. Retrieved from https://www.mayoclinic.org/dis... (access: 2020.10.10).
8.
Nikonorow E, Baraniak A, Gniadkowski M. Oporność bakterii z rodziny Enterobacteriaceae na antybiotyki β-laktamowe wynikająca z wytwarzania β-laktamaz. Post Mikrobiol. 2013; 52(3): 261–271.
9.
Gniadkowski M, Żabicka D, Hryniewicz W. Rekomendacje doboru testów do oznaczania wrażliwości bakterii na antybiotyki i chemioterapeutyki 2009: Oznaczanie wrażliwości pałeczek Gram-ujemnych. Rekomendacje KORLD 2009; 1–48. http://www.korld.edu.pl/pdf/02...] (access 2020.08.10).
10.
Evans BA, Amyes SG. OXA β-lactamases. Clin Microbiol Rev. 2014; 27(2): 241–263. doi: 10.1128/CMR.00117-13. https://doi.org/10.1128/CMR .0 0117-13.
11.
Wong JL, Evans SE. Bacterial Pneumonia in Patients with Cancer: Novel Risk Factors and Management. Clin Chest Med. 2017; 38(2): 263–277. https://doi.org/10.1016/j.ccm.....
12.
Mohanty S, Singhal R, Sood S, et al. Citrobacter infections in a tertiary care hospital in Northern India. J Infect. 2007; 54(1): 58–64. https://doi.org/10.1016/j.jinf....
13.
Rezaei M, Akya A, Elahi A, et al. The clonal relationship among the Citrobacter freundii isolated from the main hospital in Kermanshah, west of Iran. Iran J Microbiol. 2016; 8(3): 175–180.
14.
Lee CH, Lee YT, Kung CH, et al. Risk factors of community-onset urinary tract infections caused by plasmid-mediated AmpC β-lactamase-producing Enterobacteriaceae. J Microbiol Immunol Infect. 2015; 48(3): 269–275.https://doi.org/10.1016/j.jmii....
15.
Zhang R, Yang L, Cai JC, et al. High-level carbapenem resistance in a Citrobacter freundii clinical isolate is due to a combination of KPC-2 production and decreased porin expression. J Med Microbiol. 2008; 57(Pt 3): 332–337. https://doi.org/10.1099/jmm.0.....
16.
Hanson ND, Sanders CC. Regulation of inducible AmpC beta-lactamase expression among Enterobacteriaceae. Curr Pharm Des. 1999; 5(11): 881–894.
17.
Liu LH, Wang NY, Wu AY, et al. Citrobacter freundii bacteremia: Risk factors of mortality and prevalence of resistance genes. J Microbiol Immunol Infect. 2018; 51(4): 565–572. https://doi.org/10.1016/j.jmii....
18.
Rodríguez-Baño J, Gutiérrez-Gutiérrez B, Machuca I, et al. Treatment of Infections Caused by Extended-Spectrum-Beta-Lactamase-, AmpC-, and Carbapenemase-Producing Enterobacteriaceae. Clin Microbiol Rev. 2018; 31(2): e00079-17. https://doi.org/10.1128/CMR.00....
19.
Mohan S, Agarwal J, Srivastava R, Singh M. Observations on Citrobacter species from a tertiary care health center with special reference to multi-drug resistance and presence of CTX-M gene. Indian J Pathol Microbiol. 2014; 57(3): 439–441. https://doi.org/10.4103/0377-4....
20.
Greene C, Vadlamudi G, Newton D, et al. The influence of biofilm formation and multidrug resistance on environmental survival of clinical and environmental isolates of Acinetobacter baumannii. Am J Infect Control. 2016; 44(5): e65-e71.https://doi.org/10.1016/j.ajic....
21.
Michalopoulos A, Falagas ME. Treatment of Acinetobacter infections. Expert Opin Pharmacother. 2010; 11(5): 779–788.https://doi.org/10.1517/146565....
22.
Demirdal T, Sari US, Nemli SA. Is inhaled colistin beneficial in ventilator associated pneumonia or nosocomial pneumonia caused by Acinetobacter baumannii? Ann Clin Microbiol Antimicrob. 2016; 15: 11. https://doi.org/10.1186/s12941....
23.
Freire MP, de Oliveira Garcia D, Garcia CP, et al. Bloodstream infection caused by extensively drug-resistant Acinetobacter baumannii in cancer patients: high mortality associated with delayed treatment rather than with the degree of neutropenia. Clin Microbiol Infect. 2016; 22(4): 352–358.https://doi.org/10.1016/j.cmi.....
24.
Asif M, Alvi IA, Rehman SU. Insight into Acinetobacter baumannii: pathogenesis, global resistance, mechanisms of resistance, treatment options, and alternative modalities. Infect Drug Resist. 2018; 11: 1249–1260. https://doi.org/10.2147/IDR.S1....
25.
Ballouz T, Aridi J, Afif C, et al. Risk Factors, Clinical Presentation, and Outcome of Acinetobacter baumannii Bacteremia. Front Cell Infect Microbiol. 2017; 7: 156. https://doi.org/10.3389/fcimb.....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.