Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Beneficial effects of SARS-CoV-2 vaccination resulting from the COVID-19 pandemic with regard to the uptake of influenza virus, pneumococcal, and herpes zoster adult vaccination – a narrative literature review
1
MEDFIT Karolina Kłoda, Polish Society of Family Medicine, Szczecin, Poland
2
Department of Family Medicine, Pomeranian Medical University, Szczecin, Poland
3
Polish Society of Family Medicine, Department of Family Medicine, Medical University, Wrocław, Poland
Corresponding author
Artur Mierzecki
Department of Family Medicine, Pomeranian Medical University in Szczecin, Rybacka 1, 70-204, Szczecin, Poland
Department of Family Medicine, Pomeranian Medical University in Szczecin, Rybacka 1, 70-204, Szczecin, Poland
Ann Agric Environ Med. 2023;30(4):587-594
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Analysis of factors influencing COVID-19 vaccination coverage in various countries raised the question whether the recent pandemic affected the vaccination rates of other pathogens in adults. Therefore, the aim of this review article was to analyse the literature to find potentially beneficial effects of the introduction of the large-scale vaccinations resulting from the COVID-19 pandemic, with regard to the influenza virus, pneumococcal and herpes zoster adult vaccinations, in order to identify factors and strategies to increase the uptake of these vaccines.
Review methods:
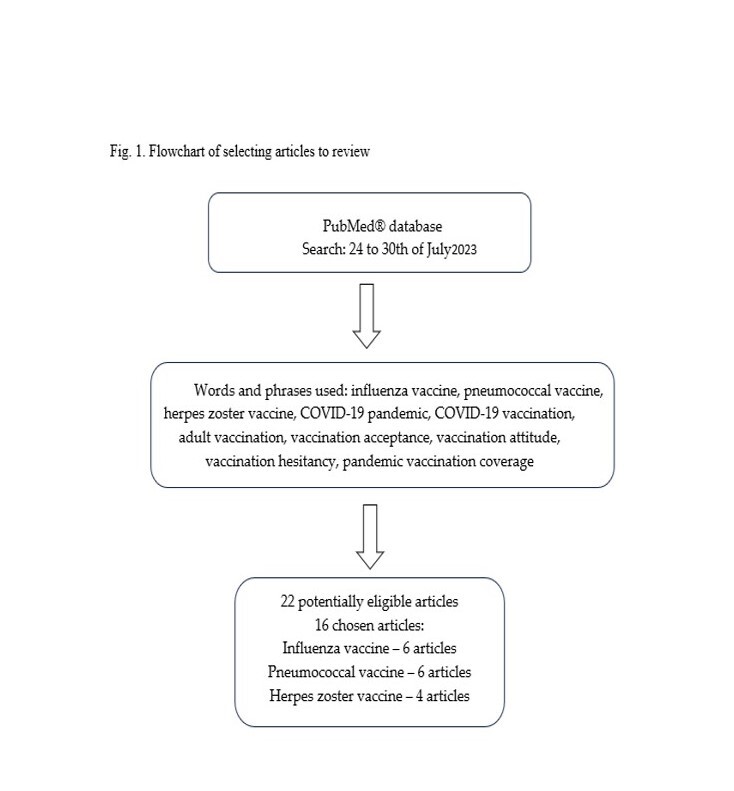
The review of the literature was based on scientific articles indexed in the PubMed Database published between 2022–2023, during the COVID-19 pandemic. Data search was performed from 24–30 July 2023.
Brief description of the state of knowledge:
It was found that the COVID-19 pandemic has had a beneficial effect on the acceptance and coverage of influenza and pneumococcal vaccination in the vulnerable elderly populations, and among healthcare workers in the case of influenza. Furthermore, the COVID-19 outbreak affected the designs of vaccine clinical trials, resulting in a lower frequency of age-related exclusion criteria, broadening the group of vaccine recipients.
Summary:
Acceptance of COVID-19 vaccination increased willingness to accept other vaccines. The attitude to vaccination is a personal decision-making process based on previous experience and interpersonal interactions, greatly affected by information and recommendation from medical professionals. The COVID-19 pandemic vaccination implementation opened new opportunities to develop prevention efforts and build vaccination strategies in middle-income countries.
Analysis of factors influencing COVID-19 vaccination coverage in various countries raised the question whether the recent pandemic affected the vaccination rates of other pathogens in adults. Therefore, the aim of this review article was to analyse the literature to find potentially beneficial effects of the introduction of the large-scale vaccinations resulting from the COVID-19 pandemic, with regard to the influenza virus, pneumococcal and herpes zoster adult vaccinations, in order to identify factors and strategies to increase the uptake of these vaccines.
Review methods:
The review of the literature was based on scientific articles indexed in the PubMed Database published between 2022–2023, during the COVID-19 pandemic. Data search was performed from 24–30 July 2023.
Brief description of the state of knowledge:
It was found that the COVID-19 pandemic has had a beneficial effect on the acceptance and coverage of influenza and pneumococcal vaccination in the vulnerable elderly populations, and among healthcare workers in the case of influenza. Furthermore, the COVID-19 outbreak affected the designs of vaccine clinical trials, resulting in a lower frequency of age-related exclusion criteria, broadening the group of vaccine recipients.
Summary:
Acceptance of COVID-19 vaccination increased willingness to accept other vaccines. The attitude to vaccination is a personal decision-making process based on previous experience and interpersonal interactions, greatly affected by information and recommendation from medical professionals. The COVID-19 pandemic vaccination implementation opened new opportunities to develop prevention efforts and build vaccination strategies in middle-income countries.
REFERENCES (50)
1.
Nehme M, Vieux L, Kaiser L, et al. The longitudinal study of subjective wellbeing and absenteeism of healthcare workers considering post-COVID condition and the COVID-19 pandemic toll. Sci Rep. 2023;13(1):10759. doi:10.1038/S41598-023-37568-1.
2.
COVID – Coronavirus Statistics – Worldometer. Accessed September 11, 2023. https://www.worldometers.info/....
3.
Kaur SP, Gupta V. COVID-19 Vaccine: A comprehensive status report. Virus Res. 2020;288. doi:10.1016/J.VIRUSRES.2020.198114.
4.
Interim analysis of COVID-19 vaccine effectiveness against Severe Acute Respiratory Infection due to SARS-CoV-2 in individuals aged 20 years and older – fourth update. Accessed September 11, 2023. https://www.ecdc.europa.eu/en/....
5.
Stolle LB, Nalamasu R, Pergolizzi J V, et al. Fact vs Fallacy: The Anti-Vaccine Discussion Reloaded. Adv Ther. 2020;37(11):4481. doi:10.1007/S12325-020-01502-Y.
6.
Klaesson J, Lobo J, Mellander C. Social interactions and COVID-19 vaccine hesitancy: Evidence from a full population study in Sweden. PLoS One. 2023 Nov 20;18(11):e0289309. doi:10.1371/journal.pone.0289309. PMID: 37983227.
7.
Khan S, Biswas MR, Shah Z. Longitudinal analysis of behavioral factors and techniques used to identify vaccine hesitancy among Twitter users: Scoping review. Hum Vaccin Immunother. 2023 Dec 15;19(3):2278377. doi:10.1080/21645515.2023.2278377. Epub 2023 Nov 20. PMID: 37981842.
8.
Aarnes RV, Nilsen MK. Norwegian Community Pharmacists’ Experiences with COVID-19 Vaccination-A Qualitative Interview Study. Pharmacy (Basel). 2023 Nov 19;11(6):181. doi:10.3390/pharmacy11060181. PMID: 37987391.
9.
Li HJ, Yang QC, Yao YY, et al. COVID-19 vaccination effectiveness and safety in vulnerable populations: a meta-analysis of 33 observational studies. Front Pharmacol. 2023;14:1144824. doi:10.3389/FPHAR.2023.1144824/BIBTEX.
10.
Roshchina Y, Rozhkova K, Roshchin S. Between nudges and mandates: The drivers of COVID-19 vaccination intentions and subsequent uptake in Russia. Vaccine. 2023;41(34):5053–5062. doi:10.1016/J.VACCINE.2023.06.067.
11.
Bhopal S, Nielsen M. Vaccine hesitancy in low- and middle-income countries: potential implications for the COVID-19 response. Arch Dis Child. 2021;106(2):113–114. doi:10.1136/ARCHDISCHILD-2020-318988.
12.
Countries with highest COVID vaccination dose rates 2023 | Statista. Accessed September 11, 2023. https://www.statista.com/stati....
13.
Hori D, Takahashi T, Ozaki A, et al. The Impact of Priority Settings at the Start of COVID-19 Mass Vaccination on Subsequent Vaccine Uptake in Japan: One-Year Prospective Cohort Study. JMIR Public Health Surveill. 2023;9. doi:10.2196/42143.
14.
Gorry C. Vaccines and Public Trust: Containing COVID-19 in Cuba. MEDICC Rev. 2022;24(1):9–13. doi:10.37757/MR2022.V24.N1.11.
15.
Cameron-Blake E, Tatlow H, Andretti B, et al. A panel dataset of COVID-19 vaccination policies in 185 countries. Nat Hum Behav. 2023;7(8). doi:10.1038/S41562-023-01615-8.
16.
Health care use – Influenza vaccination rates – OECD Data. Accessed September 13, 2023. https://data.oecd.org/healthca....
17.
Malchrzak W, Babicki M, Pokorna-Kałwak D, et al. COVID-19 Vaccination and Ukrainian Refugees in Poland during Russian–Ukrainian War—Narrative Review. Vaccines. 2022;10(6):955. doi:10.3390/VACCINES10060955.
18.
Patel UC, Schultz T, Schmidt J. Veteran influenza vaccination acceptance rates after completion of the COVID-19 vaccination series among historical influenza vaccine refusers. Vaccine. 2023;41(33). doi:10.1016/J.VACCINE.2023.06.090.
19.
Avakian I, Dadouli K, Anagnostopoulos L, et al. Nationwide Survey on Seasonal Influenza Vaccination among Health Care Workers during the COVID-19 Pandemic in Greece: Determinants, Barriers and Peculiarities. Int J Environ Res Public Health. 2023;20(13):6247. doi:10.3390/IJERPH20136247/S1.
20.
Buja A, Grotto G, Taha M, et al. Use of Information and Communication Technology Strategies to Increase Vaccination Coverage in Older Adults: A Systematic Review. Vaccines. 2023;11(7):1274. doi:10.3390/VACCINES11071274.
21.
Scudeller PG, Pereira AJ, Cerri GG, et al. Telemedicine in Brazil: Teleconsultations at the Largest University Hospital in the Country. Telemed Reports. 2023;4(1):193. doi:10.1089/TMR.2023.0012.
22.
Bhaskar S, Bradley S, Chattu VK, et al. Telemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front Public Health. 2020;8:556720. doi:10.3389/FPUBH.2020.556720.
23.
Lubomski J, Malchrzak W, Babicki M, et al. Teleconsultation as a Modern Form of Health Care Service in the Case of Poland: Assessment of Its Potential Use from the Perspective of Health Care Providers and Patients. Telemed J E Health. Published online 2023. doi:10.1089/TMJ.2023.0204.
24.
You Y, Li X, Chen B, Zou X, et al. Knowledge, Attitude, and Practice towards Influenza Vaccination among Older Adults in Southern China during the COVID-19 Pandemic. Vaccines. 2023;11(7):1197. doi:10.3390/VACCINES11071197.
25.
He R, Ren X, Huang K, et al. Influenza and pneumococcal vaccination coverage and associated factors in patients hospitalized with acute exacerbations of COPD in China: Findings from the real-world data. Chin Med J (Engl). Published online July 24, 2023. doi:10.1097/CM9.0000000000002790.
26.
Gilbert-Esparza E, Brady A, Haas S, et al. Vaccine Hesitancy in College Students. Vaccines. 2023;11(7):1243. doi:10.3390/VACCINES11071243.
27.
Inoue Y, Cooray U, Ishimaru M, et al. Oral self-care, pneumococcal vaccination, and pneumonia among Japanese older people, assessed with machine learning. Lipsitz LA, editor. J Gerontol A Biol Sci Med Sci. Published online July 10, 2023. doi:10.1093/GERONA/GLAD161.
28.
Méroc E, Fletcher MA, Hanquet G, et al. Systematic Literature Review of the Epidemiological Characteristics of Pneumococcal Disease Caused by the Additional Serotypes Covered by the 20-Valent Pneumococcal Conjugate Vaccine. Microorganisms. 2023;11(7):1816. doi:10.3390/MICROORGANISMS11071816/S1.
29.
Novaes JVLC, de Freitas Faria FM, de Bragança BSC, et al. Impacts of the COVID-19 pandemic on immunization with pneumococcal vaccines in children and older adults in Brazil. Prev Med (Baltim). 2023;173. doi:10.1016/J.YPMED.2023.107602.
30.
Filipska-Blejder K, Antczak-Komoterska A, Kostecka M, et al. Burnout Levels in Nurses and Associated Factors during the COVID-19 Pandemic—A Cross-Sectional Study. Healthcare. 2023;11(14):2032. doi:10.3390/HEALTHCARE11142032.
31.
Mateo-Gallego R, Gracia-Rubio I, Garza MC, et al. The impact of the COVID-19 pandemic in diabetes and dyslipidemia management in a Spanish region: a retrospective study of the Aragon population. Front Med. 2023;10:1191026. doi:10.3389/FMED.2023.1191026/BIBTEX.
32.
Eiden AL, DiFranzo A, Bhatti A, et al. Changes in vaccine administration trends across the life-course during the COVID-19 pandemic in the United States: a claims database study. Expert Rev Vaccines. 2023;22(1):481–494. doi:10.1080/14760584.2023.2217257.
33.
Lan C, Chen YC, Chang YI et al. Impact of COVID-19 Outbreak on Influenza and Pneumococcal Vaccination Uptake: A Multi-Center Retrospective Study. Vaccines. 2023;11(5):986. doi:10.3390/VACCINES11050986.
34.
Kalra N, Kalra T, Mishra S, et al. Hesitancy for Adult Vaccines Among Healthcare Providers and their Family Members in Delhi, India: A Cross-Sectional Study. Dialogues Health. 2022;1:100044. doi:10.1016/J.DIALOG.2022.100044.
35.
Effiong U, Umana I, Haley H, et al. Acceptance, Intent, Hesitance, and Attitudes Towards SAR-CoV-2 Vaccines Among Healthcare Workers in Michigan, USA. Cureus. 2023;15(6). doi:10.7759/CUREUS.41225.
36.
Silvonen T, Kesten J, Cabral C, et al. Views and Perceptions of People Aged 55+ on the Vaccination Programme for Older Adults in the UK: A Qualitative Study. Vaccines. 2023;11(4):870. doi:10.3390/VACCINES11040870/S1.
37.
Iwai-Saito K, Sato K, Kondo K. Associations of influenza and pneumococcal vaccinations with burdens of older family caregivers: The Japan Gerontological Evaluation study (JAGES) cross-sectional study. Vaccine. 2023;41(2):444–451. doi:10.1016/J.VACCINE.2022.11.047.
38.
Zhu J, Cole CB, Fihman J, et al. Opportunities to accelerate immunization progress in middle-income countries. Vaccine. Published online 2023. doi:10.1016/J.VACCINE.2023.06.079.
39.
Koshal SS, Ray A, Hora R, et al. Critical factors in the successful expansion of Pneumococcal Conjugate Vaccine in India during the COVID-19 pandemic. Vaccine X. 2023;14. doi:10.1016/J.JVACX.2023.100328.
40.
Bukan K, Pearce-Slade T, Eiberg M, et al. Exclusion of older adults and immunocompromised individuals in influenza, pneumococcal and COVID-19 vaccine trials before and after the COVID-19 pandemic. Aging Clin Exp Res. 2023;35(5):917–923. doi:10.1007/S40520-023-02380-4.
41.
Zhang Z, Liu X, Suo L, et al. The incidence of herpes zoster in China: A meta-analysis and evidence quality assessment. Hum Vaccin Immunother. 2023;19(2):2228169. doi:10.1080/21645515.2023.2228169.
42.
Jiang B, Wang Q, Wang Z, et al. Willingness to accept herpes zoster vaccines and the influencing factors in China. BMC Infect Dis. 2022;22(1):1–9. doi:10.1186/S12879-022-07840-2/FIGURES/1.
43.
Bennett N, Morris B, Malloy MJ, et al. An evaluation of influenza, pneumococcal and herpes zoster vaccination coverage in Australian aged care residents, 2018 to 2022. Infect Dis Heal. Published online 2023. doi:10.1016/J.IDH.2023.03.005.
44.
Domnich A, Orsi A, Ogliastro M, et al. Exploring missed opportunities for influenza vaccination and influenza vaccine co-administration patterns among Italian older adults: a retrospective cohort study. Eur J Public Health. Published online August 25, 2023:1–5. doi:10.1093/EURPUB/CKAD155.
45.
Lasagna A, Brunello A, Silvestris N et al. Italian oncologists and vaccinations against infectious diseases: Results of a survey of the Italian Association of Medical Oncology. Tumori. Published online 2023. doi:10.1177/03008916231191547.
46.
Cunniff L, Alyanak E, Fix A, et al. The impact of the COVID-19 pandemic on vaccination uptake in the United States and strategies to recover and improve vaccination rates: A review. Hum Vaccin Immunother. 2023;19(2):2246502. doi:10.1080/21645515.2023.2246502.
47.
Labuschagne LJE, Smorenburg N, van de Kassteele J, et al. Neighbourhood sociodemographic factors and COVID-19 vaccine uptake in the Netherlands: an ecological analysis. BMC Public Health. 2023;23(1):1696. doi:10.1186/S12889-023-16600-Z.
48.
Elmustafa M, Wedaa A, Babiker H, et al. Low uptake of COVID-19 vaccines in Wad Medani City, Gezira State, Sudan: Hesitancy and poor accessibility. Vaccine X. 2023;15. doi:10.1016/J.JVACX.2023.100369.
49.
Lavenue A, Simoneau I, Mahajan N, et al. Development and Implementation of Workshops to Optimize the Delivery of Vaccination Services in Community Pharmacies: Thinking beyond COVID-19. Pharm. 2023;11(4):129. doi:10.3390/PHARMACY11040129.
50.
Palache A, Billingsley JK, MacLaren K, et al. Lessons learned from the COVID-19 pandemic for improved influenza control. Vaccine. 2023;41(40). doi:10.1016/J.VACCINE.2023.08.028.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.