Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Assessment of the effect of estradiol on biochemical bone turnover markers among postmenopausal women
1
Department of Toxicology and Food Safety, Institute of Rural Health, Lublin, Poland
2
Department for Women’s Health, Institute of Rural Health, Lublin, Poland
Corresponding author
Grzegorz Raszewski
Department of Toxicology and Food Safety, Institute of Rural Health, Lublin, Poland, Jaczewskiego, 2, 20-090, Lublin, Poland
Department of Toxicology and Food Safety, Institute of Rural Health, Lublin, Poland, Jaczewskiego, 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2021;28(2):326-330
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Estrogen deficiency found in postmenopausal women may lead to disturbances in the balance of bone metabolism. Study of the influence of estradiol on markers of bone turnover may help to understand the mechanisms of bone metabolism and to monitor osteoporosis therapy in postmenopausal women at high risk of fractures. The aim of the study was evaluation of the effect of estradiol on the basic markers of bone turnover in postmenopausal women.
Material and methods:
The study was conducted in a group of 92 postmenopausal women, divided into two groups: Gr-1 with low estradiol levels ≤ 10 pg/ml and Gr-2 with reference estradiol levels ≥ 25 pg/ml). Basic markers of bone turnover were examined: Ctx (C-terminal cross-linked telopeptide of type I collagen alpha chain) and OC (osteocalcin); pro-resorptive cytokines: IL-6 and TNF-α; vitamin 25(OH)D3 and lipid profile. Women was also analyzed according to demographic and clinical data.
Results:
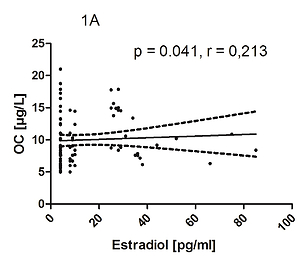
A positive relationship was found between estradiol and the main bone formation marker – OC (p = 0.041, r = 0.213) and IL-6, TNF-α (p = 0.007, r = 0.281 and p = 0.018, r = 0.246, respectivly, but only in the group with a reference hormone level. Moreover, the main markers of bone turnover: Ctx and OC showed a mutual positive correlation (p = 0.013; r = 0.257) in women with reference estradiol levels. Relationships between markers of bone remodeling, pro-resorptive cytokines and vitamin D3 depending on the level of estradiol showed no statistically significant correlation.
Conclusions:
The study showed that only in women with the reference estradiol level (≥ 25 pg/ml) were the bone formation and resorption processes balanced.
Estrogen deficiency found in postmenopausal women may lead to disturbances in the balance of bone metabolism. Study of the influence of estradiol on markers of bone turnover may help to understand the mechanisms of bone metabolism and to monitor osteoporosis therapy in postmenopausal women at high risk of fractures. The aim of the study was evaluation of the effect of estradiol on the basic markers of bone turnover in postmenopausal women.
Material and methods:
The study was conducted in a group of 92 postmenopausal women, divided into two groups: Gr-1 with low estradiol levels ≤ 10 pg/ml and Gr-2 with reference estradiol levels ≥ 25 pg/ml). Basic markers of bone turnover were examined: Ctx (C-terminal cross-linked telopeptide of type I collagen alpha chain) and OC (osteocalcin); pro-resorptive cytokines: IL-6 and TNF-α; vitamin 25(OH)D3 and lipid profile. Women was also analyzed according to demographic and clinical data.
Results:
A positive relationship was found between estradiol and the main bone formation marker – OC (p = 0.041, r = 0.213) and IL-6, TNF-α (p = 0.007, r = 0.281 and p = 0.018, r = 0.246, respectivly, but only in the group with a reference hormone level. Moreover, the main markers of bone turnover: Ctx and OC showed a mutual positive correlation (p = 0.013; r = 0.257) in women with reference estradiol levels. Relationships between markers of bone remodeling, pro-resorptive cytokines and vitamin D3 depending on the level of estradiol showed no statistically significant correlation.
Conclusions:
The study showed that only in women with the reference estradiol level (≥ 25 pg/ml) were the bone formation and resorption processes balanced.
REFERENCES (27)
1.
Rizzoli R. Postmenopausal osteoporosis: Assessment and management. Best Pract Res Clin Endocrinol Metab. 2018; 32(5): 739–57. doi.10.1016/j.beem.
2.
Janiszewska M, Barańska A, Jędrych T, Kulik T, Kasperek J, Drop B. The impact of selected factors on acceptance of illness and life satisfaction among female residents of rural areas treated for osteoporosis. Ann Agric Environ Med. 2019; 26(4): 592–599. doi.10.26444/aaem/109598.
3.
Almeida M, Laurent MR, Dubois V, et al. Estrogens and Androgens in Skeletal Physiology and Pathophysiology. Physiol Rev. 2017; 97: 135–187. doi: 10.1152/physrev.00033.2015.
4.
Katsimbri, P. The biology of normal bone remodelling. Eur J Cancer Care (Engl). 2017; 26(6): e12740. doi.10.1111/ecc.127402017.
5.
Møller AMJ, Delaissé JM, Olesen JB, et al. Aging and menopause reprogram osteoclast precursors for aggressive bone resorption. Bone Res. 2020; 8: 27. doi. 10.1038/s41413-020-0102-7.
6.
Levin VA, Jiang X, Kagan R. Estrogen therapy for osteoporosis in the modern era. Osteoporos Int. 2018; 29(5): 1049–1055. doi: 10.1007/s00198-018-4414-z.
7.
Khalid AB, Krum SA Estrogen receptors alpha and beta in bone. Bone. 2016; 87: 130–135. doi.10.1016/j.bone.2016.03.016.
8.
Almeida M, Laurent MR, Dubois V, et al. Estrogens and Androgens in Skeletal Physiology and Pathophysiology. Physiol Rev. 2017; 97: 135–18. doi: 10.1152/physrev.00033.2015.
9.
Eastell R, Szulc P. Use of bone turnover markers in postmenopausal osteoporosis. Lancet Diabetes Endocrinol. 2017; 5: 908–23. doi: 10.1016/S2213-8587(17)30184-5.
10.
Szulc P, et al. Use of CTX-I and PINP as bone turnover markers: ational Bone Health Alliance recommendations to standardize sample handling and patient preparation to reduce pre-analytical variability. Osteoporos Int. 2017; 28: 2541–56. doi: 10.1007/s00198-017-4082-4.
11.
Wheater G, Elshahaly M, Tuck SP, et al. The clinical utility of bone arker measurements in osteoporosis. J Transl Med. 2013 Aug; 11: 201. doi. 10.1186/1479-5876-11-201.
12.
Bojar I, Lyubinets O, Novotny J, et al. Intensification of menopausal ymptoms among female inhabitants of East European countries. Ann Agric Environ Med. 2016; 23(3): 517–524. doi.10.5604/12321966.1219198.
13.
Baczyk G, Chuchracki M, Klejewski A. The relationship between selected biochemical parameters, clinical factors and bone mineral density in postmenopausal women with osteoporosis. Ginekol Pol. 2012 Mar; 83 (3): 194–201.
14.
Park SG, Jeong SU, Lee JH, et al. The Changes of CTX, DPD, Osteocalcin, and Bone Mineral Density During the Postmenopausal Period. Ann Rehabil Med. 2018 Jun; 42(3): 441–448. https://doi.org/10.5535/arm.20....
15.
García-Martín A, Reyes-García R, García-Castro JM, et al. Role of serum FSH measurement on bone resorption in postmenopausal women. Endocrine. 2012 Apr; 41 (2): 302–308. https://doi.org/10.1007/s12020....
16.
Pardhe BD, Pathak S, Bhetwal A, et al. Effect of age and estrogen on biochemical markers of bone turnover in postmenopausal women: a population-based study from Nepal. Int J Womens Health. 2017; 9: 781–788. doi.org/10.2147/IJWH.S145191.
17.
Gossiel F, Finigan J, Jacques R, et al. Establishing reference intervals for bone turnover markers in healthy postmenopausal women in a nonfasting state. Bonekey Rep. 2014; 3: 573. doi.org/10.1038/bonekey.2014.68.
18.
Li C, Chen P, Duan X, et al. Bioavailable 25(OH)D but Not Total 25(OH)D Is an Independent Determinant for Bone Mineral Density in Chinese Postmenopausal Women. EBioMedicine. 2017; 15: 184–192. doi.org/10.1016/j.ebiom.2016.11.029.
19.
Naeem ST, Hussain R, Raheem A, et al. Bone Turnover Markers for Osteoporosis Status Assessment at Baseline in Postmenopausal Pakistani Females. J Coll Physicians Surg Pak. 2016 May; 26(5): 408–412.
20.
Liu Y-P, Li J, Xin S-B. Study the relevance between inflammatory factors and estradiol and their association with knee osteoarthritis in postmenopausal women. Eur Rev Med Pharmacol Sci. 2018; 22(2): 472–478. doi: 10.26355/eurrev_201801_14197.
21.
Malutan AM, Dan M, Nicolae C, Carmen M. Proinflammatory and anti-inflammatory cytokine changes related to menopause. Prz Menopauzalny. 2014; 13(3): 162–8. doi: 10.5114/pm.2014.43818.
22.
Chen YN, Wei P, Yu Bs J. Higher concentration of serum C-terminal cross-linking telopeptide of type I collagen is positively related with inflammatory factors in postmenopausal women with H-type hypertension and osteoporosis. Orthop Surg. 2019; 11(6): 1135–1141. https://doi.org/10.1111/os.125....
23.
Kocka KH, Ślusarska BJ, Nowicki GJ, et al. Level of vitamin 25 (OH) D and B group vitamins and functional efficiency among the chronically ill elderly in domiciliary care – a pilot study. Ann Agric Environ Med. 2019; 26(3): 489–495. doi: 10.26444/aaem/105801.
24.
Pop LC, Shapses SA, Chang B, et al. Vitamin D-binding protein in healthy pre- and postmenopausal women: relationship with estradiol concentrations. Endocr Pract. 2015 Aug; 21 (8): 936–942. https://doi.org/10.4158/EP1562....
25.
Guney G, Sener-Simsek B, Tokmak A, et al. Assessment of the Relationship between Serum Vitamin D and Osteocalcin Levels with Metabolic Syndrome in Non-Osteoporotic Postmenopausal Women. Geburtshilfe Frauenheilkd. 2019 Mar; 79(03): 293–299. https://doi.org/10.1055/a-0767....
26.
Al-Daghri NM, Yakout S, Al-Shehri E, et al. Inflammatory and bone turnover markers in relation to PTH and vitamin D status among Saudi postmenopausal women with and without osteoporosis. Int J Clin Exp Med. 2014 Sep 15; 7(9): 2812–2819.
27.
Schwetz V, Trummer C, Pandis M, et al. Effects of Vitamin D Supplementation on Bone Turnover Markers: A Randomized Controlled Trial. Nutrients. 2017; 9(5): 432. https://doi.org/10.3390/nu9050....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.