Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Assessment of functional capacity of the elderly
1
ORPEA POLAND, Warsaw, Poland
2
Institute of Environmental Protection – National Research Institute, Warsaw, Poland
3
Institute of Rural Health, Lublin, Poland
4
Collegium Medicum, Jan Kochanowski University, Kielce, Poland
5
Faculty of Pedagogy and Psychology, Jan Kochanowski University, Kielce, Poland
6
Department of Internal Nursing, Faculty of Health Sciences, Medical University, Wrocław, Poland
Corresponding author
Magdalena Florek-Łuszczki
Instytut Medycyny Wsi w Lublinie, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Instytut Medycyny Wsi w Lublinie, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2023;30(1):156-163
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Ageing is a continuous, progressive process of functional reserve loss. Physical fitness and mental state have a significant impact on the functionality level of the elderly population. Assessing the degree elderly people’s of independence regarding self-care is an important aspect of the Comprehensive Geriatric Assessment (CGA). The aim of the study was to assess the functional capacity of people over 65 years of age.
Material and methods:
The study involved 312 patients in hospital wards across Lower Silesia, south-west Poland. The criteria for participation were as follows: providing informed consent to participate in the study, intellectual capacity to be interviewed, and age over 65. The study applied the diagnostic survey method, together with the use of the VAS, Barthel, IADL and GDS scales.
Results:
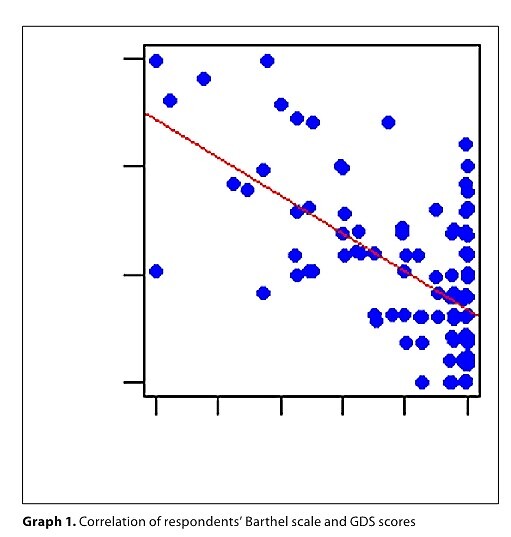
Among the respondents, 59.94% were in a moderately severe condition according to the Barthel scale, average IADL score – 20.56 points; according to the GDS scale, 58.97% had no symptoms of depression. Respondents suffered from multiple chronic diseases, the most common of which were hypertension (71.47%); they also reported some medical issues, mainly back pain (47.44). Assessment of the correlation of the Barthel and GDS scales, as well as the IADL and GDS, revealed a significant and negative correlation at -0.49 and -0.50. Assessment of the correlation between the number of diseases and the Barthel scale was -0.49, the number of symptoms and the Barthel scale -0.4; pain severity and the Barthel scale -0.41, number of diseases and IADL -0.58, and number of symptoms and IADL -0.52.
Conclusions:
The greater the seniors’ independence regarding instrumental activities of daily living, the weaker the symptoms of depression. Multimorbidity and experiencing pain impaired independence among the elderly.
Ageing is a continuous, progressive process of functional reserve loss. Physical fitness and mental state have a significant impact on the functionality level of the elderly population. Assessing the degree elderly people’s of independence regarding self-care is an important aspect of the Comprehensive Geriatric Assessment (CGA). The aim of the study was to assess the functional capacity of people over 65 years of age.
Material and methods:
The study involved 312 patients in hospital wards across Lower Silesia, south-west Poland. The criteria for participation were as follows: providing informed consent to participate in the study, intellectual capacity to be interviewed, and age over 65. The study applied the diagnostic survey method, together with the use of the VAS, Barthel, IADL and GDS scales.
Results:
Among the respondents, 59.94% were in a moderately severe condition according to the Barthel scale, average IADL score – 20.56 points; according to the GDS scale, 58.97% had no symptoms of depression. Respondents suffered from multiple chronic diseases, the most common of which were hypertension (71.47%); they also reported some medical issues, mainly back pain (47.44). Assessment of the correlation of the Barthel and GDS scales, as well as the IADL and GDS, revealed a significant and negative correlation at -0.49 and -0.50. Assessment of the correlation between the number of diseases and the Barthel scale was -0.49, the number of symptoms and the Barthel scale -0.4; pain severity and the Barthel scale -0.41, number of diseases and IADL -0.58, and number of symptoms and IADL -0.52.
Conclusions:
The greater the seniors’ independence regarding instrumental activities of daily living, the weaker the symptoms of depression. Multimorbidity and experiencing pain impaired independence among the elderly.
ACKNOWLEDGEMENTS
The study was financed under the programme of the Ministry
of Education and Science in Warsaw in 2019–2023 under
the title: ‘Regional Initiative of Excellence’ (Project No. 024/
RID/2018/19).
REFERENCES (43)
1.
Oliveira A, Nossa P, Mota-Pinto A. Assessing Functional Capacity and Factors Determining Functional Decline in the Elderly: A Cross-Sectional Study. Acta Med Port. 2019;32(10):654–660. https://doi.org/10.2034/amp.11....
2.
Ćwirlej-Sozańska AB, Wiśniowska-Szurlej A, Wilmowska-Pietruszyńska A, et al. Factors associated with disability and quality of life among the oldest-old living in community in Poland – a cross-sectional study. Ann Agric Environ Med. 2020;27(4):621–629. https://doi.org/10.26444/aaem/....
3.
Błachnio A, Buliński L. Wellbeing and older adults in primary health care in Poland. Ann Agric Environ Med. 2019;26(1):55–61. https://doi.org/10.26444/aaem/....
4.
Lutomski P, Kaczoruk M, Florek-Łuszczki M. Ageing policy in Poland during the COVID-19 pandemic. Ann Agric Environ Med. 2021;28(4):551–557. https://doi.org/doi:10.26444/a....
5.
Kumięga P, Grata-Borkowska U, Bujnowska-Fedak M, et al. Całościowa ocena geriatryczna a opieka medyczna nad osobą w wieku podeszłym. Puls Uczelni. 2016;2(10):44–48. https://doi.org/doi:10.5604/20....
6.
Pilotto A, Cella A, Pilotto A, et al. Three Decades of Comprehensive Geriatric Assessment: Evidence Coming From Different Healthcare Settings and Specific Clinical Conditions. Journal of American Medical Directors Association. 2017;18(2):192.e1–192.e11. https://doi.org/doi:10.1016/j.....
7.
Wolf D, Rhein C, Geschke K, et al. Preventable hospitalizations among older patients with cognitive impairments and dementia. International Psychogeriatrics. 2019;31(3):383–391. https://doi.org/doi:10.1017/S1....
8.
McPhee JS, French DP, Jackson D, et al. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17(3):567–580. https://doi.org/doi:10.1007/s1....
9.
Slot RER, Sikkes SAM, Berkhof J, et al. Subjective cognitive decline and rates of incident Alzheimer’s disease and non-Alzheimer’s disease dementia. Alzheimers Dement. 2019;15(3):465–476. https://doi.org/doi:10.1016/j.....
10.
Liang YJ, Su QW, Sheng ZR, et al. Effectiveness of Physical Activity Interventions on Cognition, Neuropsychiatric Symptoms, and Quality of Life of Alzheimer’s Disease: An Update of a Systematic Review and Meta-Analysis. Front Aging Neurosci. 2022;14:830824. https://doi.org/doi:10.3389/fn....
11.
Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Arch Phys Med Rehabil. 2004;85:1694–1704.
12.
Czarkowska M, Saran T, Mazur A, et al. Comprehensive outpatient rehabilitation increases the ability of people over 60 to live independently. Ann Agric Environ Med. 2018;25(4):720–724. https://doi.org/doi:10.26444/a....
13.
Girzelska J, Głowacka M, Wilk-Jeziorska D, et al. Profilaktyka samotności i osamotnienia jako czynnik determinujący zdrowie seniora. Pielegniarstwo XXI wieku/Nursing in the 21st Century. 2018;17(4):41–46. https://doi.org/doi:10.2478/pi....
14.
Ćwirlej-Sozańska AB, Sozański B, Wiśniowska-Szurlej A, et al. Quality of life and related factors among older people living in rural areas in south-eastern Poland. Ann Agric Environ Med. 2018;25(3):539–545. https://doi.org/doi:10.26444/a....
15.
Hoogendijk EO, Afilalo J, Ensrud KE, et al. Frailty: implications for clinical practice and public health. The Lancet. 2019;394(10206):1365–1375. https://doi.org/doi:10.1016/S0....
16.
Starczewska M, Prociak L, Markowska A, et al. Ocena sprawności funkcjonalnej osób w podeszłym wieku, Problemy Pielęgniarstwa. 2018;26(3):222–227. https://doi.org/doi:10.5114/pp....
17.
Bogusz R, Charzyńska-Gula M, Szkuat M, et al. Sprawność funkcjonalna osób powyżej 70. roku życia na wsi a zapotrzebowanie na opiekę. Med. Og Nauk Zdr. 2013;19(4):517–522.
18.
Prodinger B, O’Connor RJ, Stucki G, et al. Establishing score equivalence of the Functional Independence Measure motor scale and the Barthel Index, utilising the International Classification of Functioning, Disability and Health and Rasch measurement theory. J Rehabil Med. 2017;49(5):416–422. https://doi.org/doi:10.2340/16....
19.
Babiarczyk B, Schlegel-Zawadzka M, Turbiarz A. Ocena częstości występowania objawów depresji w populacji osób powyżej 65. roku życia. Med Og Nauk Zdr. 2013;19(4):453–457.
20.
Fidecki W, Wysokiński M, Wrońska I, et al. Ocena ryzyka depresji wśród osób starszych ze środowiska wiejskiego. Geriatria. 2019;13:147–151.
21.
Kowalska J, Szczepańska-Gieracha J, Piątek J. Zaburzenia poznawcze i emocjonalne a długość pobytu osób starszych w Zakładzie Opiekuńczo-Leczniczym o Profilu Rehabilitacyjnym. Pszchogeraitr Pol. 2010; 7(2):61–70.
22.
Kok R, Reynolds ChF. Management of Depression in Older Adults: A Review. JAMA 2017;317(20):2114–2122. https://doi.org/doi:10.1001/ja....
23.
Boulton ER, Horne M, Todd C. Multiple influences on participating in physical activity in older age: Developing a social ecological approach. Health Expect. 2017;21(1):239–248. https://doi.org/doi:10.1111/he....
24.
Knyszyńska A, Radecka A, Bryczkowska I, et al. Związek pomiędzy sprawnością funkcjonalną a poziomem depresji wśród mieszkańców Domów Pomocy Społecznej. Gerontol Pol. 2019;27:144–149.
25.
Leyland L-A, Spencer B, Beale N, et al. The effect of cycling on cognitive function and well-being in older adults. PLoS ONE. 2019;14(2):e0211779. https://doi.org/doi:10.1371/jo....
26.
Notthoff, N, Carstensen LL. Positive messaging promotes walking in older adults. Psychology and Aging. 2014;29(2):329–341. https://doi.org/doi:10.1037/a0....
27.
Rybka M, Rezmerska L, Haor B. Ocena sprawności osób w wieku podeszłym. Zeszyty Naukowe WSHE. 2016;2(1):4–12. https://doi.org/doi:10.19251/p...).
28.
Fidecki W, Wysokiński M, Kulina D, et al. Assessment of the functional efficiency of the elderly. Pol J Public Health. 2021;130(1):45–47. https://doi.org/doi:10.2478/pj....
29.
Maresova P, Javanmardi E, Barakovic S, et al. Consequences of chronic diseases and other limitations associated with old age – a scoping review. BMC Public Health. 2019;19:1431. https://doi.org/doi:10.1186/s1....
30.
Bektas A, Schurman SH, Sen R, el al. Aging, inflammation and the environment. Experimental Gerontology. 2018;105:10–18. https://doi.org/doi:10.1016/j.....
31.
Bączyk G, Kozłowska K, Samborski W. Jakość życia uwarunkowana stanem zdrowia chorych na reumatoidalne zapalenie stawów—przegląd piśmiennictwa. Forum Reumatol. 2017;3(4):222–229.
32.
Chatterji S, Byles J, Cutler D, et al. Health, functioning, and disability in older adults—present status and future implications. The Lancet. 2019;385(9967):563–575. https://doi.org/doi:10.1016/S0....
33.
Ajayi SA, Adebusoye LA, Ogunbode AM, et al. Profile and correlates of functional status in elderly patients presenting at a primary care clinic in Nigeria. Afr J Prim Health Care Fam Med. 2015;7(1):810. https://doi.org/doi:10.4102/ph....
34.
Mone P, Gambardella J, Lombardi A, et al. Correlation of physical and cognitive impairment in diabetic and hypertensive frail older adults. Cardiovasc Diabetol. 2022;21:10. https://doi.org/doi:10.1186/s1....
35.
Gomes GC, Teixeira-Salmela LF, Fonseca BE, et al. Age and education influence the performance of elderly women on the dual-task Timed Up and Go test. Arq Neuropsiquiatr. 2015;73:187–193. https://doi.org/doi:10.1590/00....
36.
Busch TA, Duarte YA, Nunes DP, et al. Factors associated with lower gait speed among the elderly living in a developing country: a cross-sectional population-based study. BMC Geriatrics. 2015;15:35. https://doi.org/doi:10.1186/s1....
37.
Vieira ER, Palmer RC, Chaves PH. Prevention of falls in older people living in the community. BMJ. 2016;353:i1419. https://doi.org/doi:10.1136/bm....
38.
Sherrington C, Tiedemann A. Physiotherapy in the prevention of falls in older people. J Physiol. 2015;61(2):54–60. https://doi.org/doi:10.1016/j.....
39.
Misztal-Okońska P, Młynarska M, Goniewicz M, et al. Polipragmazja wśród osób po 65 roku życia. J Educat Health Sport. 2017;7(8):267–279. https://doi.org/doi:10.5281/ze....
40.
Blanco-Reina E, Ariza-Zafra G, Ocana-Riola R, et al. 2012 American Geriatrics Society Beers criteria: enhanced applicability for detecting potentially inappropriate medications in European older adults? A comparison with the Screening Tool of Older Person’s Potentially Inappropriate Prescriptions. J Am Geriatr Soc. 2014;62(7):1217–1223. https://doi.org/doi:10.1111/jg....
41.
Awad A, Hanna O. Potentially inappropriate medication use among geriatric patients in primary care setting: A cross-sectional study using the Beers, STOPP, FORTA and MAI criteria. PloS ONE. 2019;14(6):e0218174. https://doi.org/doi:10.1371/jo....
42.
Fang EF, Xie C, Schenkel JA, et al. A research agenda for ageing in China in the 21st century (2nd edition): Focusing on basic and translational research, long-term care, policy and social networks. Ageing Res Rev. 2020;101174. https://doi.org/doi:10.1016/j.....
43.
Zhou Y, Li Y, Zhu X, et al. Medical and Old-Age Care Integration Model and Implementation of the Integrated Care of Older People (ICOPE) in China: Opportunities and Challenges. J Nutr Health Aging. 2021;25: 720–723. https://doi.org/doi:10.1007/s1....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.