Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Bleeding during pregnancy as a reason for interventions by emergency medical services teams in Poland
1
Medical University, Warsaw, Poland
2
Medical University, Lublin, Poland
Ann Agric Environ Med. 2022;29(1):110-114
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Vaginal bleeding during pregnancy is associated with risks to the health and life of the woman and/or the foetus. Moreover, it is usually unanticipated, which requires on-site care to be provided to the woman. Such care is handled by emergency medical services (EMS) teams until specialist obstetric care can be provided. The purpose of study was to analyze the characteristics of EMS team responses to calls regarding pregnant women with vaginal bleeding, considering the location of call: urban vs. rural area.
Material and methods:
The study was based on a retrospective analysis of 5,487 EMS team interventions due to vaginal bleeding in pregnant women in Poland. The data analyzed included the period January 2018-December 2019, obtained from the National Monitoring Centre of Emergency Medical Services.
Results:
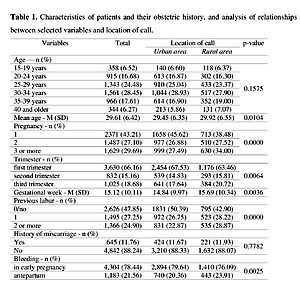
The teams were more commonly dispatched to pregnant women in rural areas, who were more likely to be older and in the course of a second (27.52% vs. 26.88%) or subsequent pregnancy (34.00% vs. 27.49%), to have had one (28.22% vs. 26.75%) or more previous births (28.87% vs. 22.87%), and to have antepartum bleeding (23.91% vs. 20.36%) than those from urban areas. The mean time between receipt of the call and patient hand-over at the hospital by the EMS team was longer in rural areas (50.00 vs. 37.23 minutes).
Conclusions:
EMS teams responding to calls from rural areas regarding pregnant women with vaginal bleeding were most commonly dispatched in the summer, and the mean time between the receipt of the call and patient hand-over at the hospital was longer than in the calls from urban areas. Compared to patients calling from urban areas, those from rural areas were also more likely to be pregnant for the second or subsequent time, to have antepartum bleeding, and to have given birth before.
Vaginal bleeding during pregnancy is associated with risks to the health and life of the woman and/or the foetus. Moreover, it is usually unanticipated, which requires on-site care to be provided to the woman. Such care is handled by emergency medical services (EMS) teams until specialist obstetric care can be provided. The purpose of study was to analyze the characteristics of EMS team responses to calls regarding pregnant women with vaginal bleeding, considering the location of call: urban vs. rural area.
Material and methods:
The study was based on a retrospective analysis of 5,487 EMS team interventions due to vaginal bleeding in pregnant women in Poland. The data analyzed included the period January 2018-December 2019, obtained from the National Monitoring Centre of Emergency Medical Services.
Results:
The teams were more commonly dispatched to pregnant women in rural areas, who were more likely to be older and in the course of a second (27.52% vs. 26.88%) or subsequent pregnancy (34.00% vs. 27.49%), to have had one (28.22% vs. 26.75%) or more previous births (28.87% vs. 22.87%), and to have antepartum bleeding (23.91% vs. 20.36%) than those from urban areas. The mean time between receipt of the call and patient hand-over at the hospital by the EMS team was longer in rural areas (50.00 vs. 37.23 minutes).
Conclusions:
EMS teams responding to calls from rural areas regarding pregnant women with vaginal bleeding were most commonly dispatched in the summer, and the mean time between the receipt of the call and patient hand-over at the hospital was longer than in the calls from urban areas. Compared to patients calling from urban areas, those from rural areas were also more likely to be pregnant for the second or subsequent time, to have antepartum bleeding, and to have given birth before.
REFERENCES (38)
1.
King TL, Davidson MR, Avery CD, et al. Anatomy and physiology of pregnancy: placental, fetal, and maternal adaptations. In: King TL, Brucker MC, Kriebs JM, Fahey JO, Gegor CL, Varney H, editors. Varney’s Midwifery. 5th ed. Jones & Bartlett Learning; 2015. p. 599–627.
2.
Rashad WA, Essa RM. Women’s Awareness of Danger Signs of Obstetrics Complications. J Am Sci. 2010; 6(10): 1299–1306. doi:10.7537/marsjas061010.149.
3.
Nowacka E, Światek-Zdzienicka M, Jarzębski R. Stany zagrożenia życia w położnictwie. Anest Inten Terap. 2004; 36: 286–292.
4.
Mwilike B, Nalwadda G, Kagawa M, et al. Knowledge of danger signs during pregnancy and subsequent healthcare seeking actions among women in Urban Tanzania: a cross-sectional study. BMC Pregnancy Childbirth. 2018; 18(1): 4. doi: 10.1186/s12884-017-1628-6.
5.
Gregory DS, Wu V, Tuladhar P. The Pregnant Patient: Managing Common Acute Medical Problems. Am Fam Physician. 2018; 98(9): 595–602.
6.
Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019; 99(3): 166–174.
7.
Hasan R, Baird DD, Herring AH, et al. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol. 2010; 20(7): 524–31. doi: 10.1016/j.annepidem.2010.02.006.
9.
Knez J, Day A, Jurkovic D. Ultrasound imaging in the management of bleeding and pain in early pregnancy. Best Pract Res Clin Obstet Gynaecol. 2014; 28(5): 621–36. doi: 10.1016/j.bpobgyn.2014.04.003.
10.
Ticconi C, Pietropolli A, Specchia M, et al. Pregnancy-Related Complications in Women with Recurrent Pregnancy Loss: A Prospective Cohort Study. J Clin Med. 2020; 9(9): 2833. doi: 10.3390/jcm9092833.
11.
Yang J, Savitz DA, Dole N, et al. Predictors of vaginal bleeding during the first two trimesters of pregnancy. Paediatr Perinat Epidemiol. 2005; 19(4): 276–83. doi: 10.1111/j.1365-3016.2005.00655.x.
12.
Young JS, White LM. Vaginal Bleeding in Late Pregnancy. Emerg Med Clin North Am. 2019; 37(2): 251–264. doi: 10.1016/j.emc.2019.01.006.
13.
Sakornbut E, Leeman L, Fontaine P. Late pregnancy bleeding. Am Fam Physician. 2007; 75(8): 1199–206.
14.
Li Y, Tian Y, Liu N, et al. Analysis of 62 placental abruption cases: Risk factors and clinical outcomes. Taiwan J Obstet Gynecol. 2019; 58(2): 223–226. doi: 10.1016/j.tjog.2019.01.010.
15.
Downes KL, Grantz KL, Shenassa ED. Maternal, Labor, Delivery, and Perinatal Outcomes Associated with Placental Abruption: A Systematic Review. Am J Perinatol. 2017; 34(10): 935–957. doi: 10.1055/s-0037-1599149.
16.
Raj SS, Manthri S, Sahoo PK. Emergency referral transport for maternal complication: lessons from the community based maternal death audits in Unnao district, Uttar Pradesh, India. Int J Health Policy Manag. 2015; 4(2): 99–106. doi: 10.15171/ijhpm.2015.14.
17.
Ustawa z dnia 8 września 2006 r. o Państwowym Ratownictwie Medycznym (Dz.U. 2019 poz. 993).
18.
System Wspomagania Dowodzenia Państwowego Ratownictwa Medycznego (SWD PRM) https://www.gov.pl/web/zdrowie...- (access: 12.02.2021).
19.
Ananth CV, Oyelese Y, Prasad V, et al. Evidence of placental abruption as a chronic process: associations with vaginal bleeding early in pregnancy and placental lesions. Eur J Obstet Gynecol Reprod Biol. 2006; 128(1–2): 15–21. doi: 10.1016/j.ejogrb.2006.01.016.
20.
Hossain R, Harris T, Lohsoonthorn V, et al. Risk of preterm delivery in relation to vaginal bleeding in early pregnancy. Eur J Obstet Gynecol Reprod Biol. 2007; 135(2): 158–63. doi: 10.1016/j.ejogrb.2006.12.003.
21.
Sapra KJ, Joseph KS, Galea S, et al. Signs and Symptoms of Early Pregnancy Loss. Reprod Sci. 2017; 24(4): 502–513. doi: 10.1177/1933719116654994.
22.
Lykke JA, Dideriksen KL, Lidegaard O, et al. First-trimester vaginal bleeding and complications later in pregnancy. Obstet Gynecol. 2010; 115(5): 935–944. doi: 10.1097/AOG.0b013e3181da8d38.
23.
Magnus MC, Wilcox AJ, Morken NH, et al. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019; 364: l869. doi: 10.1136/bmj.l869.
24.
Ghimire PR, Akombi-Inyang BJ, Tannous C, et al. Association between obesity and miscarriage among women of reproductive age in Nepal. PLoS One. 2020; 15(8): e0236435. doi: 10.1371/journal.pone.0236435.
25.
du Fossé NA, van der Hoorn MP, van Lith JMM, et al. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: a systematic review and meta-analysis. Hum Reprod Update. 2020; 26(5): 650–669. doi: 10.1093/humupd/dmaa010.
26.
San Lazaro Campillo I, Meaney S, Sheehan J, et al. University students’ awareness of causes and risk factors of miscarriage: a cross-sectional study. BMC Womens Health. 2018; 18(1): 188. doi: 10.1186/s12905-018-0682-1.
27.
Feodor Nilsson S, Andersen PK, Strandberg-Larsen K, et al. Risk factors for miscarriage from a prevention perspective: a nationwide follow-up study. BJOG. 2014; 121(11): 1375–84. doi: 10.1111/1471-0528.12694.
28.
Singh S, Doyle P, Campbell OMR, et al. Pregnant women who requested a ‘108’ ambulance in two states of India. BMJ Glob Health. 2018; 3(3): e000704. doi: 10.1136/bmjgh-2017-000704.
29.
Bills CB, Newberry JA, Darmstadt G, et al. Reducing early infant mortality in India: results of a prospective cohort of pregnant women using emergency medical services. BMJ Open. 2018; 8(4): e019937. doi: 10.1136/bmjopen-2017-019937.
30.
Singh S, Doyle P, Campbell OM, et al. Interfacility transfer of pregnant women using publicly funded emergency call centre-based ambulance services: a cross-sectional analysis of service logs from five states in India. BMJ Open. 2017; 7(6): e015077. doi: 10.1136/bmjopen-2016-015077.
31.
Strehlow MC, Newberry JA, Bills CB, et al. Characteristics and outcomes of women using emergency medical services for third-trimester pregnancy-related problems in India: a prospective observational study. BMJ Open. 2016; 6(7): e011459. doi: 10.1136/bmjopen-2016-011459.
32.
Cantwell K, Burgess S, Morgans A, et al. Temporal trends in falls cases seen by EMS in Melbourne: The effect of residence on time of day and day of week patterns. Injury. 2016; 47(1): 266–71. doi: 10.1016/j.injury.2015.10.073.
33.
Faramand Z, Frisch SO, Martin-Gill C, et al. Diurnal, weekly and seasonal variations of chest pain in patients transported by emergency medical services. Emerg Med J. 2019; 36(10): 601–607. doi: 10.1136/emermed-2019-208529.
34.
Ramgopal S, Dunnick J, Owusu-Ansah S, et al. Weather and Temporal Factors Associated with Use of Emergency Medical Services. Prehosp Emerg Care. 2019; 23(6): 802–810. doi: 10.1080/10903127.2019.1593563.
35.
Javaudin F, Hamel V, Legrand A, et al. Unplanned out-of-hospital birth and risk factors of adverse perinatal outcome: findings from a prospective cohort. Scand J Trauma Resusc Emerg Med. 2019; 27(1): 26. doi: 10.1186/s13049-019-0600-z.
36.
Rzońca P, Gałązkowski R, Wójcik-Fatla A, et al. Missions of the Helicopter Emergency Medical Service in rural and urban areas in Poland – A comparative retrospective analysis. Ann Agric Environ Med. 2019; 26(2): 355–360. doi:10.26444/aaem/106223.
37.
Rzońca P, Świeżewski SP, Jalali R, et al. Helicopter Emergency Medical Service (HEMS) Response in Rural Areas in Poland: Retrospective Study. Int J Environ Res Public Health. 2019; 16(9): 1532. doi: 10.3390/ijerph16091532.
38.
Dechert TA, Sarani B, McMaster M, et al. Medical emergency team response for the non-hospitalized patient. Resuscitation. 2013; 84(3): 276–9. doi: 10.1016/j.resuscitation.2012.06.022.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.