Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Relationship between periodontal diseases and non-specific inflammatory bowel diseases – an overview. Part I
1
Institute of Rural Health, Lublin, Poland
2
Student of the Faculty of Medicine and Dentistry, Jagiellonian University Medical College, Kraków, Poland
3
Higher School of Health Promotion, Kraków, Poland
Corresponding author
Ann Agric Environ Med. 2024;31(1):1-7
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
An increasing number of studies indicate that the oral cavity and gastrointestinal tract are interconnected and that there is a potential causal link between non-specific inflammatory bowel diseases (IBD) and oral diseases. Therefore, following the example of the brain-gut axis, the concept of the gum-gut axis has now been put forward. The aim of the review is to assess the literature confirming the existence of the recently proposed gum-gut axis and the resulting relationships between non-specific inflammatory bowel diseases and oral diseases, especially periodontal diseases.
Review methods:
The review sums-up information concerning the relationship between periodontal diseases and non-specific bowel diseases. A literature review was carried out by searching databases PubMed, Google Scholar, and Web of Science.
Brief description of the state of knowledge:
Previously, it was presumed that oral microflora and intestinal microflora remain separate. because it was considered that salivary microbes are killed by stomach and bile acids during translocation through the gastrointestinal tract. Presently, it has been confirmed that oral microorganisms have been found in the faeces of even healthy people. The comparison of oral and intestinal microbiomes of adults does not show full convergence; but pathogenic bacteria such as Klebsiella, Porphyromonas gingivalis and Fusobacterium nucleatum may act as the microbial bridge between periodontitis and IBD.
Summary:
Dysbiosis of oral microflora may disrupt the normal functioning of the immune system, in this way increasing the development of periodontitis which, in turn, increases the risk of IBD and other complex systemic pathological processes. The gum-gut axis plays a crucial role in these associations. Additional studies are necessary to specify the role of nutritional intervention concerning oral and intestinal microbiome for precise health management.
An increasing number of studies indicate that the oral cavity and gastrointestinal tract are interconnected and that there is a potential causal link between non-specific inflammatory bowel diseases (IBD) and oral diseases. Therefore, following the example of the brain-gut axis, the concept of the gum-gut axis has now been put forward. The aim of the review is to assess the literature confirming the existence of the recently proposed gum-gut axis and the resulting relationships between non-specific inflammatory bowel diseases and oral diseases, especially periodontal diseases.
Review methods:
The review sums-up information concerning the relationship between periodontal diseases and non-specific bowel diseases. A literature review was carried out by searching databases PubMed, Google Scholar, and Web of Science.
Brief description of the state of knowledge:
Previously, it was presumed that oral microflora and intestinal microflora remain separate. because it was considered that salivary microbes are killed by stomach and bile acids during translocation through the gastrointestinal tract. Presently, it has been confirmed that oral microorganisms have been found in the faeces of even healthy people. The comparison of oral and intestinal microbiomes of adults does not show full convergence; but pathogenic bacteria such as Klebsiella, Porphyromonas gingivalis and Fusobacterium nucleatum may act as the microbial bridge between periodontitis and IBD.
Summary:
Dysbiosis of oral microflora may disrupt the normal functioning of the immune system, in this way increasing the development of periodontitis which, in turn, increases the risk of IBD and other complex systemic pathological processes. The gum-gut axis plays a crucial role in these associations. Additional studies are necessary to specify the role of nutritional intervention concerning oral and intestinal microbiome for precise health management.
REFERENCES (70)
1.
Sheng JA, Bales NJ, Myers SA, Bautista AI, Roueinfar M, Hale TM, Handa RJ. The hypothalamic-pituitary-adrenal axis: development, programming actions of hormones, and maternal-fetal interactions. Front Behav Neurosci. 2021;14:256.
2.
Leistner C, Menke A. Hypothalamic–pituitary–adrenal axis and stress. Handbook Clin Neurol. 2020;175:55–64.
3.
DeMorrow S. Role of the Hypothalamic-Pituitary-Adrenal Axis in Health and Disease. Int J Mol Sci. 2018 Mar 26;19(4):986. doi:10.3390/ijms19040986. PMID: 29587417; PMCID: PMC5979578.
4.
Dinan TG, Gryan JD The mictrobiote Gut-Brain-Axix in health and disease Gastrenterol. 2017;46:77–89.
5.
Mayer EA, Nance K, Chen S. The Gut–Brain Axis. Annual Rev Med. 2022;73:439–453.
6.
Brzozowski B, Mazur-Bialy A, Pajdo R, Kwiecien S, Bilski J, Zwolinska-Wcislo M, Brzozowski T. Mechanisms by which stress affects the experimental and clinical inflammatory bowel disease (IBD): role of brain-gut axis. Curr Neuropharmacol. 2016;14(8):892–900.
7.
Xu Y, Luo J, Gao Y, Tao Y, Xu J, Yao T, Chen Y. Causal effects between inflammatory bowel disease and oral diseases based on Oral-GUT Axis: a Mendelian randomization study. Nutrients 2023;15(20):4445 https://doi.org/10.3390/nu1520....
8.
Byrd KM, Gulati AS. The “Gum-Gut” Axis in Inflammatory Bowel Diseases: A Hypothesis-Driven Review of Associations and Advances. Front Immunol. 2021 Feb 19;12:620124. doi:10.3389/fimmu.2021.620124. PMID: 33679761; PMCID: PMC7933581.
9.
Baima G, Ribaldone DG, Romano F, Aimetti M, Romandini M. The Gum–Gut Axis: Periodontitis and the Risk of Gastrointestinal Cancers. Cancers 2023;15(18):4594.
10.
Schneider S, WrightCM, Heuckeroth RO. Unexpected Roles for the Second Brain: Enteric Nervous System as Master Regulator of Bowel Function. Annual Rev Physiol. 2019;81:235–259.
11.
Schmidt TS, Hayward MR, Coelho LP, Li SS, Costea PI, Voigt AY, et al. Extensive Transmission of Microbes along the Gastrointestinal Tract. ELife 2019;8:e42693.
12.
Nagao J-I, Kishikawa S, Tanaka H, Toyonaga K, Narita Y, Negoro-Yasumatsu K, et al. Pathobiont-Responsive Th17 cells in gut-mouth axis provoke inflammatory oral disease and are modulated by intestinal microbiome. Cell Rep. 2022;40:111314.
13.
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104(34):13780–5. doi:10.1073/pnas.0706625104. Epub 2007 Aug 15. PMID: 17699621; PMCID: PMC1959459.
14.
Meyle J, Chapple I. Molecular aspects of the pathogenesis of periodontitis. Periodontol 2000. 2015 Oct;69(1):7–17. doi:10.1111/prd.12104. PMID: 26252398.
15.
Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers 2017;3:17038. doi:10.1038/nrdp.2017.38.
16.
Chapple ILC, Mealey BL, Van Dyke TE, Bartold PM, Dommisch H, Eickholz P, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018 Jun;89 Suppl 1:S74-S84. doi:10.1002/JPER.17-0719. PMID: 29926944.
17.
Isola G, Santonocito S, Distefano A, Polizzi A, Vaccaro M, Raciti G, et al. Impact of periodontitis on gingival crevicular fluid miRNAs profiles associated with cardiovascular disease risk. J Periodontal Res. 2022;58(1):165–174.
18.
Genco RJ, Sanz M. Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontol 2000. 2020;83:7–13. doi:10.1111/prd.12344.
19.
Möller B, Kollert F, Sculean A, Villiger PM. Infectious triggers in periodontitis and the gut in rheumatoid arthritis (RA): A complex story about association and causality. Front Immunol. 2020;11. doi:10.3389/fimmu.2020.01108.
20.
Torrealba-García D, Garcia-Morales P, Torrealba E, Cejudo JC, Silvestre-Rangil J. Is there a relationship between periodontitis and alzheimer’s disease? systematic review and comparative analysis. Alzheimers Dement. 2021;17:e051470. doi:10.1002/alz.051470.
21.
Koirala PK, Pradhan S. Gold Standards in Periodontics: A Review. J Nepalese Soc Periodontol Oral Implantol. 2021;5(1):49–53.
22.
Zhou T, Xu W, Wang Q, Jiang C, Li H, Chao Y, Sun Y, A L. The effect of the “Oral-Gut” axis on periodontitis in inflammatory bowel disease: A review of microbe and immune mechanism associations. Front Cell Infect Microbiol. 2023;13:1132420. doi:10.3389/fcimb.2023.1132420. PMID: 36923589; PMCID: PMC10008960.
23.
Baima G, Muwalla M, Testa G, Mazza F, Bebars A, Perotto S, et al. Periodontitis prevalence and severity in inflammatory bowel disease: A case–control study. J Periodontol. 2022:1–10. doi:10.1002/jper.22-0322.
24.
Imai J, Ichikawa H, Kitamoto S, Golob JL, Kaneko M, Nagata J, et al. A potential pathogenic association between periodontal disease and crohn’s disease. JCI Insight 2021;6:e148543. doi:10.1172/jci.insight.148543.
25.
Zhang Y, Qiao D, Chen R, Zhu F, Gong J, Yan F. The association between periodontitis and inflammatory bowel disease: A systematic review and meta-analysis. BioMed Res Int. 2021:1–8. doi:10.1155/2021/6692420.
27.
Petagna L, Antonelli A, Ganini C, Bellato V, Campanelli M, Divizia A, et al. Pathophysiology of Crohn’s disease inflammation and recurrence. Biol Direct. 2020;15(1):1–10.
28.
Caparrós E, Wiest R, Scharl M, Rogler G, Gutiérrez Casbas A, Yilmaz B, et al. Dysbiotic microbiota interactions in Crohn’s disease. Gut Microbes 2021;13(1):1949096.
29.
Turpin W, Lee SH, Garay JAR, Madsen KL, Meddings JB, Bedrani L, et al. Increased intestinal permeability is associated with later development of Crohn’s disease. Gastroenterol. 2020;159(6):2092–2100.
30.
Kaczmarczyk O, Dąbek-Drobny A, Woźniakiewicz M, Paśko P, Dobrowolska-Iwanek J, Woźniakiewicz A, et al. Association between fecal levels of short-chain fatty acids and serum pro-and anti-Inflammatory cytokines in patients with inflammatory bowel disease. Folia Medica Cracoviensia. 2022:43–54.
31.
Segal JP, LeBlanc JF, Hart AL. Ulcerative colitis: an update. Clin Med. 2021;21(2):135.
32.
Raine T, Bonovas S, Burisch J. ECCO guidelines on the therapeutics in ulcerative colitis: medical treatment. J Crohns Colitis. 2022;16:2–17.
33.
Eder P, Łodyga M, Gawron-Kiszka M, et al. Guidelines for the management of ulcerative colitis. Recommendations of the Polish Society of Gastroenterology and the Polish National Consultant in Gastroenterology. Gastroenterol Rev. 2023;18:1–42.
34.
She Y, Kong X, Ge Y, Liu Z, Chen J, Jiang J, et al. Periodontitis and inflammatory bowel disease: a meta-analysis. BMC Oral. Health. 2020;20:67. doi:10.1186/s12903-020-1053-5.
35.
Jairath V, Feagan BG. Global burden of inflammatory bowel disease. Lancet Gastroenterol Hepatol. 2020;5(1):2–3.
36.
Marotto D, Atzeni F, Ardizzone S, Monteleone G, Giorgi V, Sarzi-Puttini P. Extra-intestinal manifestations of inflammatory bowel diseases. Pharmacol Res. 2020;161:105206. doi:10.1016/j.phrs.2020.105206.
37.
Chi YC, Chen JL, Wang LH, Chang K, Wu CL, Lin SY, et al. Increased risk of periodontitis among patients with Crohn’s disease: a population-based matched-cohort study. Int J Colorectal Dis. 2018;33:1437 44. doi:10.1007/s00384-018-3117-4.
38.
Lin CY, Tseng KS, Liu JM, Chuang HC, Lien CH, Chen YC, et al. Increased risk of ulcerative colitis in patients with periodontal disease: a nationwide population-based cohort study. Int J Environ Res Public Health. 2018;15:602. doi:10.3390/ijerph15112602.
39.
Kang EA, Chun J, Kim JH, Han K, Soh H, Park S, et al. Periodontitis combined with smoking increases risk of the ulcerative colitis: a national cohort study. World J Gastroenterol. 2020;26:5661–72. doi:10.3748/wjg.v26.i37.5661.
40.
Machado V, Lobo S, Proença L, Mendes JJ, Botelho J. Vitamin d and periodontitis: A systematic review and meta-analysis. Nutrients. 2020;12:2177. doi:10.3390/nu12082177.
41.
Liu H, Hong XL, Sun TT, Huang XW, Wang JL, Xiong H. Fusobacterium nucleatum exacerbates colitis by damaging epithelial barriers and inducing aberrant inflammation. J Dig Dis. 2020;21:385–398. doi:10.1111/1751-2980.12909.
42.
Zhang Y, Chen J, Fu H, Kuang S, He F, Zhang M, et al. Exosomes derived from 3D-cultured MSCs improve therapeutic effects in periodontitis and experimental colitis and restore the Th17 cell/Treg balance in inflamed periodontium. Int J Oral Sci. 2021;13:43. doi:10.1038/s41368-021-00150-4.
43.
Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14:573 84. doi:10.1038/nrgastro.2017.88.
44.
Franzosa EA, Sirota-Madi A, Avila-Pacheco J, Fornelos N, Haiser HJ, Reinker S, et al. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Nat Microbiol. 2019;4:293–305. doi:10.1038/s41564-018-0306-4.
45.
Lavelle A, Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2020;17:223–237. doi:10.1038/s41575-019-0258.
46.
Lee Y-C, Liu C-Y, Lee C-L, Zhang R-H, Huang C-J, Yen T-L. The periodontopathic pathogen, porphyromonas gingivalis, involves a gut inflammatory response and exacerbates inflammatory bowel disease. Pathogens 2022;11:84. doi:10.3390/pathogens11010084.
47.
Cai Z, Zhu T, Liu F, Zhuang Z, Zhao L. Co-pathogens in Periodontitis and Inflammatory Bowel Disease. Front Med. 2021;8:723719. doi:10.3389/fmed.2021.723719.
48.
Curtis MA, Diaz PI, Van Dyke TE. The role of the microbiota in periodontal disease. Periodontology. 2020;83(1):14–25. doi:10.1111/prd.12296.
49.
Reyes L. Porphyromonas gingivalis. Trends Microbiol. 2021;29:376–377. doi: 10.1016/j.tim.2021.01.010.
50.
Xu W, Zhou W, Wang H, Liang S. Roles of porphyromonas gingivalis and its virulence factors in periodontitis. Adv Protein Chem Struct Biol. 2020;120:45–84. doi:10.1016/bs.apcsb.2019.12.001.
51.
Wei Y, Shi M, Nie Y, Wang C, Sun F, Jiang W, et al. Integrated analysis of the salivary microbiome and metabolome in chronic and aggressive periodontitis: A pilot study. Front. Microbiol. 2022;13. doi:10.3389/fmicb.2022.959416.
52.
Matsuoka K, Kanai T. The gut microbiota and inflammatory bowel disease. Semin Immunopathol. 2014;37:47–55. doi:10.1007/s00281-014-0454-4.
53.
Guan Q. A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. 2019:7247238. doi:10.1155/2019/7247238.
54.
Nishida A, Inoue R, Inatomi O, Bamba S, Naito Y, Andoh A. Gut microbiota in the pathogenesis of inflammatory bowel disease. J Clin Gastroenterol. 2018;11(1):1–10. doi:10.1007/s12328-017-0813-5.
55.
Dolan KT, Chang EB. Diet, gut microbes, and the pathogenesis of inflammatory bowel diseases. Molecular Nutrition Food Res. 2017;61(1) doi:10.1002/mnfr.201600129.
56.
Andrzejewska M, Dereziński P, Kokot ZJ, Grzymisławski M. Metabolomika i proteomika w diagnostyce nieswoistych chorób zapalnych jelit. Forum Zaburzeń Metabolicznych. 2016;7(4):145–151.
57.
Schmidt TS, Hayward MR, Coelho LP, Li SS, Costea PI, Voigt AY, et al. Extensive transmission of microbes along the gastrointestinal tract. eLife 2019; 8:e42693. doi:10.7554/eLife.42693.
58.
Newman KL, Kamada N. Pathogenic associations between oral and gastrointestinal diseases. Trends Mol Med. 2022;28:1030–1039. doi:10.1016/j.molmed.2022.05.006.
59.
Jia L, Wu R, Han N, Fu J, Luo Z, Guo L, et al. Porphyromonas gingivalis and Lactobacillus rhamnosus GG regulate the Th17/Treg balance in colitis via TLR4 and TLR2. Clin Transl Immunology. 2020;9:e1213. 10.1002/cti2.1213.
60.
Huh JW, Roh TY. Opportunistic detection of Fusobacterium nucleatum as a marker for the early gut microbial dysbiosis. BMC Microbiol. 2020;20:208. 10.1186/s12866-020-01887-4.
61.
Gemmell MR, Berry S, Mukhopadhya I, Hansen R, Nielsen HL, Bajaj-Elliott M, et al. Comparative genomics of Campylobacter concisus: analysis of clinical strains reveals genome diversity and pathogenic potential. Emerg Microbes Infect. 2018;7:116. 10.1038/s41426-018-0118-x.
62.
Kitamoto S, Nagao-Kitamoto H, Jiao Y, Gillilland MG, Hayashi A, Imai J, et al. The intermucosal connection between the mouth and gut in commensal pathobiont-driven colitis. Cell. 2020;182:447–62.e14.10.1016/j.cell.2020.05.048.
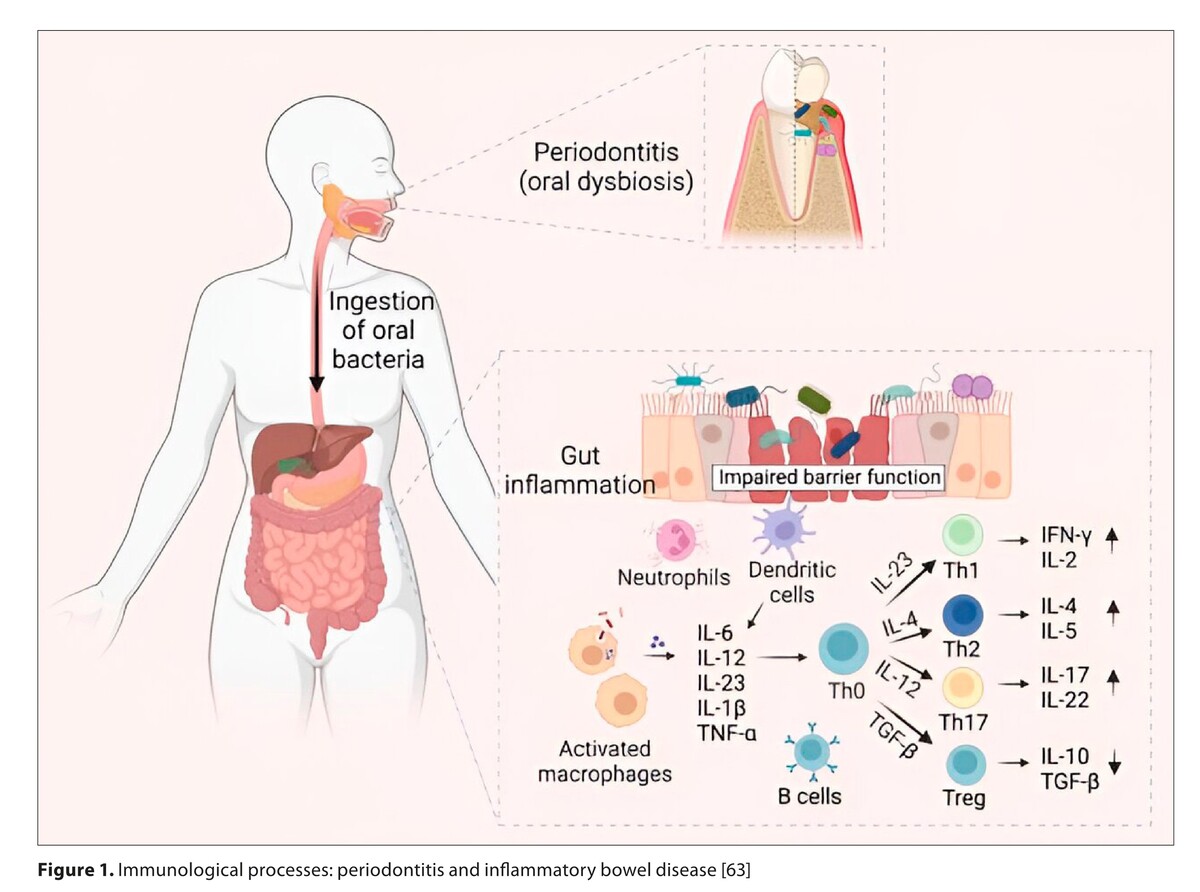
63.
Tanwar H, Gnanasekaran JM, Allison D, Chuang LS, He X, Aimetti M, Baima G, et al. Unraveling the Link between Periodontitis and Inflammatory Bowel Disease: Challenges and Outlook. ArXiv 2023 Aug 19:arXiv:2308.10907v1. PMID: 37645044; PMCID: PMC10462160.
64.
Jaeger N, Gamini R, Cella M, Schettini JL, Bugatti M, Zhao S, et al. Single-cell analyses of Crohn’s disease tissues reveal intestinal intraepithelial T cells heterogeneity and altered subset distributions. Nat Commun. 2021;12:1921. doi:10.1038/s41467-021-22164-6.
65.
Read E, Curtis MA, Neveres JF. Oral pathogen-mediated immune responses that drive gut inflammation in IBD. Nature Rev Gastroenterol Hepatol. 2021;18:731–742.
66.
Yang B, Pang X, Li Z, Chen Z, Wang Y. Immunomodulation in the treatment of periodontitis: Progress and perspectives. Front Immunol. 2021;12. doi:10.3389/fimmu.2021.781378.
67.
Gugnani S, Gugnani N. Is there any link between periodontitis and inflammatory bowel diseases? Evid Based Dent. 2023 Sep;24(3):127–129. doi:10.1038/s41432-023-00917-0. Epub 2023 Jul 20. PMID: 37474731.
68.
Yuan X, Zhou F, Wang H, Xu X, Xu S, Zhang C, et al. Systemic antibiotics increase microbiota pathogenicity and oral bone loss. Int J Oral Sci. 2023;15:4. doi:10.1038/s41368-022-00212-1.
69.
Figueredo CM, Martins AP, Lira-Junior R, Menegat JB, Carvalho AT, Fischer RG, et al. Activity of inflammatory bowel disease influences the expression of cytokines in gingival tissue. Cytokine. 2017;95:1–6. doi:10.1016/j.cyto.2017.01.016/ijms24119577.
70.
Lauritano D, Boccalari E, Di Stasio D, Della Vella F, Carinci F, Lucchese A, et al. Prevalence of oral lesions and correlation with intestinal symptoms of inflammatory bowel disease: a systematic review. Diagnostics (Basel). 2019;9:77. doi:10.3390/diagnostics9030077.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.