Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
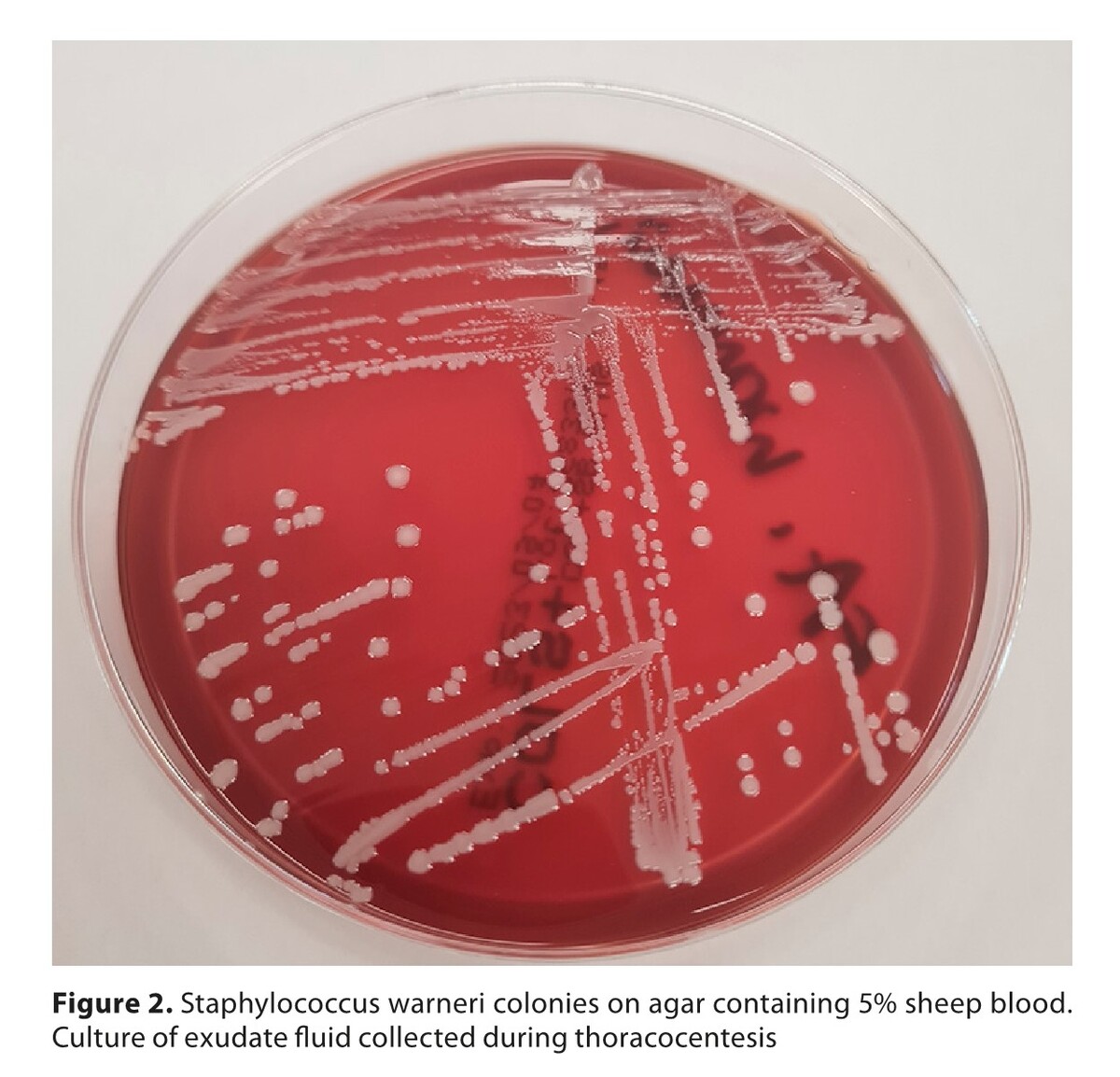
A case of exudative pleuritis caused by Staphylococcus warneri
1
Stefan Cardinal Wyszyński District Specialist Hospital, Lublin, Poland
2
Department of Human Anatomy, Medical University, Lublin, Poland
Corresponding author
Małgorzata Maria Skiba
Stefan Cardinal Wyszyński District Specialist Hospital, Kraśnicka 100, 20-718, Lublin, Poland
Stefan Cardinal Wyszyński District Specialist Hospital, Kraśnicka 100, 20-718, Lublin, Poland
Ann Agric Environ Med. 2024;31(3):442-445
KEYWORDS
TOPICS
- Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)
- Prevention of occupational diseases in agriculture, forestry, food industry and wood industry
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
This paper discusses the case of a patient with exudative bacterial pneumonia caused by Staphylococcus warneri. The patient had been abusing alcohol and nicotine for several decades, which should be considered an immunosuppressive factor. Staphylococcus warneri is part of the skin microbiome, but can also be a pathogenic agent in certain circumstances. Pleural fluid is an unusual site of isolation for the staphylococcus described. The literature contains case reports of arthritis, endocarditis, urinary tract infection or infection associated with continuous ambulatory peritoneal dialysis caused by Staphylococcus warneri. With the development of medicine, the phenomenon of immunosuppression is becoming more common, posing the threat of an increase in invasive infections caused by coagulase-negative staphylococci. In addition, an overly liberal use of antibiotics may contribute to the generation of multidrug resistance in these micro-organisms.
REFERENCES (36)
1.
Welch WH. Conditions underlying the infection of wounds. Am J Med Sci. 1891:439–465.
2.
Qi S, Gao B, Zhu S. A Fungal Defensin Inhibiting Bacterial Cell-Wall Biosynthesis with Non-Hemolysis and Serum Stability. J Fungi. 2022;8(2):174. https://doi.org/10.3390/jof802....
3.
Kloos WE, Bannerman TL. Update on clinical significance of coagulase-negative staphylococci. Clin Microbiol Rev. 1994;7(1):117–140. https://doi.org/10.1128/cmr.7.....
4.
Heilmann C, Ziebuhr W, Becker K. Are coagulase-negative staphylococci virulent? Clin Microbiol Infect. 2019;25(9):1071–1080. https://doi.org/10.1016/j.cmi.....
5.
Paranthaman K, Wilson A, Verlander N, et al. Trends in coagulase-negative staphylococci (CoNS), England, 2010–2021. Access Microbiol. 2023;5(6):acmi000491.v3. https://doi.org/10.1099/acmi.0....
6.
França A. The Role of Coagulase-Negative Staphylococci Biofilms on Late-Onset Sepsis: Current Challenges and Emerging Diagnostics and Therapies. Antibiotics. 2023;12(3):554. https://doi.org/10.3390/antibi....
7.
Pinheiro-Hubinger L, Moraes Riboli DF, Abraao LM, et al. Coagulase-Negative Staphylococci Clones Are Widely Distributed in the Hospital and Community. Pathogens. 2021;10(7):792. https://doi.org/10.3390/pathog....
8.
Shin JH, Kim SH, Jeong HS, et al. Identification of coagulase-negative staphylococci isolated from continuous ambulatory peritoneal dialysis fluid using 16S ribosomal RNA, tuf, and SodA gene sequencing. Perit Dial Int. 2011;31(3):340–346. https://doi.org/10.3747/pdi.20....
9.
Bertelloni F, Cagnoli G, Bresciani F, et al. Antimicrobial Resistant Coagulase-Negative Staphylococci Carried by House Flies (Musca domestica) Captured in Swine and Poultry Farms. Antibiotics (Basel). 2023;12(4):636. https://doi.org/10.3390/antibi....
10.
Becker K, Both A, Weißelberg S, et al. Emergence of coagulase-negative staphylococci. Expert Rev Anti Infect Ther. 2020;18(4):349–366. https://doi.org/10.1080/147872....
11.
Michels R, Last K, Becker SL, et al. Update on Coagulase-Negative Staphylococci-What the Clinician Should Know. Microorganisms. 2021;9(4):830. https://doi.org/10.3390/microo....
12.
Ansari F, Banerjee T, Kumar A, et al. Coagulase-Negative Staphylococci in Neonatal Blood: How Concerning? J Lab Physicians. 2023;15(1):126–130. https://doi.org/ 10.1055/s-0042-1757411.
13.
Popa-Fotea NM, Scafa-Udriste A, Iulia G, et al. Increasing clinical impact and microbiological difficulties in diagnosing coagulase-negative staphylococci in infective endocarditis – a review starting from a series of cases. Curr Med Res Opin. 2022;38(12):2077–2083. https://doi.org/10.1080/030079....
14.
Yamamoto J, Endo A, Sugawara H, et al. Native Valve Endocarditis due to Staphylococcus warneri Developing in a Patient with Type 1 Diabetes. Intern Med. 2020;59(18):2269–2274. https://doi.org/10.2169/intern....
15.
Żukowska A, Hryniewicz W, editors. Recommendations for diagnosis, therapy and antibiotic prophylaxis of infections in hospital – 2020, Material for therapeutic committees and antibiotic therapy teams. National Medicines Institute 2020. [in Polish].
16.
Kern A, Perreten V. Clinical and molecular features of methicillin-resistant, coagulase-negative staphylococci of pets and horses. J Antimicrob Chemother. 2013;68(6):1256–1266. https://doi.org/10.1093/jac/dk....
17.
de Oliveira RP, da Silva JG, Aragao BB, et al. Diversity and emergence of multi-resistant Staphylococcus spp. isolated from subclinical mastitis in cows in of the state of Piauí, Brazil. Braz J Microbiol. 2022;53:2215–2222. https://doi.org/10.1007/s42770....
18.
Regecová I, Výrostková J, Zigo F, et al. Detection of Resistant and Enterotoxigenic Strains of Staphylococcus warneri Isolated from Food of Animal Origin. Foods. 2022;11(10):1496. https://doi.org/10.3390/foods1....
19.
Wang M, Wang C, Yang C, et al. Effects of Lactobacillus plantarum C7 and Staphylococcus warneri S6 on flavor quality and bacterial diversity of fermented meat rice, a traditional Chinese food. Food Res Int. 2021; 150(Pt A):110745. https://doi.org/10.1016/j.food....
20.
Lawal OU, Adekanmbi AO, Adelowo OO. Occurrence of methicillin-resistant staphylococci in the pig-production chain in Ibadan, Nigeria. Onderstepoort J Vet Res. 2021;88(1):e1-e4. https://doi.org/10.4102/ojvr.v....
21.
Abdel-Moein KA, Zaher HM. The Nasal Carriage of Coagulase-Negative Staphylococci Among Animals and Its Public Health Implication. Vector-Borne Zoonotic Dis. 2020;20(12):897–902. http://doi.org/10.1089/vbz.202....
22.
Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870–926. https://doi.org/10.1128/cmr.00....
23.
Şimşek F, Yevgi R, Yalçin A. Primary Bacterial Ventriculitis caused by Staphylococcus warneri. Rev Soc Bras Med Trop. 2023;56:e0631. https://doi.org/10.1590/0037-8....
24.
Stöllberger C, Wechsler-Fördös A, Geppert F, et al. Staphylococcus warneri endocarditis after implantation of a lumbar disc prosthesis in an immunocompetent patient. J Infect. 2006;52(1):15–18. https://doi.org/10.1016/j.jinf....
25.
Diaconu R, Golumbeanu E, Constantin A, et al. Native valve endocarditis with Staphylococcus warneri. BMJ Case Rep. 2019;12(6):e229546. http://dx.doi.org/10.1136/bcr-....
26.
Alawad MJ, Ali GA, Goravey W. Underrecognized pathogen; Staphylococcus warneri-associated native mitral valve endocarditis in an immunocompetent host: A case report and literature review. Clin Case Rep. 2022;10(4):e05591. https://doi.org/10.1002/ccr3.5....
27.
Gelman R, Potruch A, Oster Y, et al. Native aortic valve Staphylococcus warneri endocarditis after COVID-19 infection: a case report and a review of literature. APMIS. 2022;130(5):270–275. https://doi.org/10.1111/apm.13....
28.
Kurihara I, Yoshida K, Fukuchi T, et al. Native mitral valve infective endocarditis caused by Staphylococcus warneri: A case-based review. Clin Case Rep. 2021;9:e0476. https://doi.org/10.1002/ccr3.4....
29.
Albert NM, Bena JF, Ciudad C, et al. Contamination of reusable electroencephalography electrodes: A multicenter study. Am J Infect Control. 2018;46(12):1360–1364. https://doi.org/10.1016/j.ajic....
30.
Kanuparthy A, Challa T, Meegada S, et al. Staphylococcus warneri: Skin Commensal and a Rare Cause of Urinary Tract Infection. Cureus. 2020;12(5):e8337. https://doi.org/10.7759/cureus....
31.
Björkqvist M, Liljedahl M, Zimmermann J, et al. Colonization pattern of coagulase-negative staphylococci in preterm neonates and the relation to bacteremia. Eur J Clin Microbiol Infect Dis. 2010;29(9):1085–1093. https://doi.org/10.1007/s10096....
32.
Battisti O, Mitchison R, Davies PA. Changing blood culture isolates in a referral neonatal intensive care unit. Arch Dis Child. 1981;56:775–778. http://dx.doi.org/10.1136/adc.....
33.
Heilmann C, Ziebuhr W, Becker K. Are coagulase-negative staphylococci virulent? Clin Microbiol Infect. 2019;25(9):1071–80. https://doi.org/10.1016/j.cmi.....
34.
Rouard C, Doucet-Populaire F, Guillet-Caruba C, et al. Deletion of One 23S rRNA Gene (rrl) Copy Contributes to the Development of Linezolid Resistance in Staphylococcus warneri. Antimicrob Agents Chemother. 2018;62(11):e01139–18. https://doi.org/10.1128/aac.01....
35.
Colombo APV, do Souto RM, Araújo LL, et al. Antimicrobial resistance and virulence of subgingival staphylococci isolated from periodontal health and diseases. Sci Rep 2023; 13(1):11613 (2023). https://doi.org/10.1038/s41598....
36.
Friedrich AW. Control of hospital acquired infections and antimicrobial resistance in Europe: the way to go. Wien Med Wochenschr. 2019; 169(1):25–30. https://doi.org/10.1007/s10354....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.