Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Translation and psychometric testing of the Polish version of the Neonatal Extent of Work Rationing Instrument (NEWRI)
1
Department of Paediatrics, Faculty of Health Sciences, Medical University, Wrocław, Poland
2
Department of Clinical Nursing, Faculty of Health Sciences, Medical University, Wrocław, Poland
Corresponding author
Anna Rozensztrauch
Department of Pediatrics, Faculty of Health Sciences, Wrocław Medical University, Wrocław, Poland, Bartla 5, 51-618, Wroclaw, Poland
Department of Pediatrics, Faculty of Health Sciences, Wrocław Medical University, Wrocław, Poland, Bartla 5, 51-618, Wroclaw, Poland
Ann Agric Environ Med. 2021;28(1):94-98
KEYWORDS
psychometric evaluationPolish validation studyneonatal nursingcare rationingNeonatal Extent of Work Rationing Instrument
TOPICS
ABSTRACT
Objective:
The aim of the study was to perform translation and cultural adaptation, as well as to assess the validity and reliability of the Polish version of the Neonatal Extent of Work Rationing Instrument (NEWRI) questionnaire for evaluating care rationing in neonatal intensive care units (NICUs) in Poland.
Material and methods:
Participants were prospectively recruited at the University Clinical Hospital in Wroclaw, Poland, and the study conducted from January 2018 – June 2018. The adaptation process involved translation of survey items following the guidelines for cross-cultural translation and evaluation of psychometric properties, as well as an assessment of construct validity, reliability, and internal consistency of the NEWRI using Cronbach’s alpha.
Results:
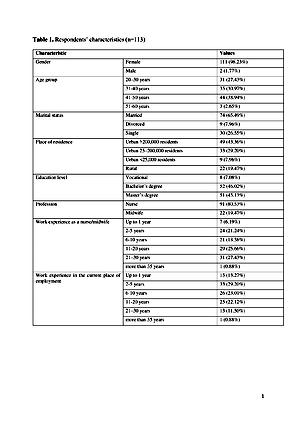
113 professionally active nurses (n=90) and midwives (n=23) were enrolled in the study. Cronbach’s alpha for the entire instrument was 0.982. Results for subscales: life support and technology-oriented nursing care – Cronbach’s alpha – 0.95, parental support and teaching and infant comfort care – 0.95, patient surveillance – 0.92, care coordination and discharge planning – 0.79. All items of the questionnaire were found to have a positive discriminatory power.
Conclusions:
The present findings indicate a high level of reliability and validity of the translated questionnaire, fully comparable to that of the original. The questionnaire can be used for evaluating care rationing in NICUs.
The aim of the study was to perform translation and cultural adaptation, as well as to assess the validity and reliability of the Polish version of the Neonatal Extent of Work Rationing Instrument (NEWRI) questionnaire for evaluating care rationing in neonatal intensive care units (NICUs) in Poland.
Material and methods:
Participants were prospectively recruited at the University Clinical Hospital in Wroclaw, Poland, and the study conducted from January 2018 – June 2018. The adaptation process involved translation of survey items following the guidelines for cross-cultural translation and evaluation of psychometric properties, as well as an assessment of construct validity, reliability, and internal consistency of the NEWRI using Cronbach’s alpha.
Results:
113 professionally active nurses (n=90) and midwives (n=23) were enrolled in the study. Cronbach’s alpha for the entire instrument was 0.982. Results for subscales: life support and technology-oriented nursing care – Cronbach’s alpha – 0.95, parental support and teaching and infant comfort care – 0.95, patient surveillance – 0.92, care coordination and discharge planning – 0.79. All items of the questionnaire were found to have a positive discriminatory power.
Conclusions:
The present findings indicate a high level of reliability and validity of the translated questionnaire, fully comparable to that of the original. The questionnaire can be used for evaluating care rationing in NICUs.
ACKNOWLEDGEMENTS
The authors express their thanks to all respondents for their
contributions in this research. Certified English language
services were provided by a highly qualified academic native
English speaker. The authors also thank Dr. Christian
M. Rochefort for sharing the original version of NEWRI
instrument.
FUNDING
This study was conducted under a research project funded by
the Ministry of Science and Higher Education of Poland as a
part of a statutory grant of the Wroclaw Medical University
for maintaining research potential (no. SUB.E020.19.003).
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
There were no other contributors to the article than the
authors, nor was there any assistance in writing the study.
REFERENCES (23)
1.
Trajkovski S, Schmied V, Vickers M, Jackson D. Neonatal nurses’ perspectives of family-centred care: a qualitative study. J Clin Nurs. 2012 Sep; 21(17–18): 2477–87.
2.
Alderdice F, Gargan P, McCall E, Franck L. Online information for parents caring for their premature baby at home: A focus group study and systematic web search. Health Expect. 2018 Aug; 21(4): 741–51.
3.
Kalisch BJ. Missed nursing care: a qualitative study. J Nurs Care Qual. 2006 Dec; 21(4): 306–13; quiz 314–5.
4.
Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008 Aug; 20(4): 227–37.
5.
Schubert M, Clarke SP, Aiken LH, de Geest S. Associations between rationing of nursing care and inpatient mortality in Swiss hospitals. Int J Qual Health Care. 2012 Jun; 24(3): 230–8.
6.
Kalisch BJ, Xie B, Dabney BW. Patient-reported missed nursing care correlated with adverse events. Am J Med Qual. 2014 Oct; 29(5): 415–22.
7.
Carthon JMB, Lasater KB, Sloane DM, Kutney-Lee A. The quality of hospital work environments and missed nursing care is linked to heart failure readmissions: a cross-sectional study of US hospitals. BMJ Qual Saf. 2015 Apr; 24(4): 255–63.
8.
Larcher V, Craig F, Bhogal K, Wilkinson D, Brierley J, Royal College of Paediatrics and Child Health. Making decisions to limit treatment in life-limiting and life-threatening conditions in children: a framework for practice. Arch Dis Child. 2015 May; 100 Suppl 2: s3–23.
9.
Papastavrou E, Andreou P, Vryonides S. The hidden ethical element of nursing care rationing. Nurs Ethics. 2014 Aug; 21(5): 583–93.
10.
Scheunemann LP, White DB. The Ethics and Reality of Rationing in Medicine. Chest. 2011 Dec; 140(6): 1625–32.
11.
Scott PA, Harvey C, Felzmann H, Suhonen R, Habermann M, Halvorsen K, et al. Resource allocation and rationing in nursing care: A discussion paper. Nurs Ethics. 2019; 26(5): 1528–39.
12.
Griffiths P, Recio‐Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, et al. The association between nurse staffing and omissions in nursing care: A systematic review. J Adv Nurs. 2018 Jul; 74(7): 1474–87.
13.
Rochefort CM, Clarke SP. Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. J Adv Nurs. 2010 Oct; 66(10): 2213–24.
14.
Rochefort CM, Rathwell BA, Clarke SP. Rationing of nursing care interventions and its association with nurse-reported outcomes in the neonatal intensive care unit: a cross-sectional survey. BMC Nurs. 2016; 15: 46.
15.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000 Dec 15; 25(24): 3186–91.
16.
Gjersing L, Caplehorn JR, Clausen T. Cross-cultural adaptation of research instruments: language, setting, time and statistical considerations. BMC Med Res Methodol. 2010 Feb 10; 10: 13.
17.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing [Internet]. Vienna, Austria; 2017. Available from: https://www.R-project.org/.
18.
Ferreira MBG, Haas VJ, Dantas RAS, Felix MM dos S, Galvão CM. Cultural adaptation and validation of an instrument on barriers for the use of research results 1. Rev Lat Am Enfermagem [Internet]. 2017 Mar 9 [cited 2019 Jan 16];25. Available from: https://www.ncbi.nlm.nih.gov/p....
19.
Schubert M, Glass TR, Clarke SP, Schaffert-Witvliet B, De Geest S. Validation of the Basel Extent of Rationing of Nursing Care instrument. Nurs Res. 2007 Dec; 56(6): 416–24.
20.
Jones TL. Validation of the Perceived Implicit Rationing of Nursing Care (PIRNCA) instrument. Nurs Forum. 2014 Jun; 49(2): 77–87.
21.
Schmalenberg C, Kramer M. Types of intensive care units with the healthiest, most productive work environments. Am J Crit Care. 2007 Sep; 16(5): 458–68; quiz 469.
22.
Manojlovich M, Laschinger HKS. Application of the Nursing Worklife Model to the ICU setting. Crit Care Nurs Clin North Am. 2008 Dec; 20(4): 481–7.
23.
Beaton D, Bombardier C, Guillemin F, Ferraz M. Recommendations for the Cross-Cultural Adaptation of the DASH & QuickDASH Outcome Measures. 2nd ed. Toronto, Canada: Institute for Work & Health; 2007.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.